Journal Menu
Articles
Useful links
- Peer Review
- Why Submit?
- Submission Checklist
- Article Types
- Instructions for Authors
- Article Processing Fee
Home Menu
Laparoscopic Removal of the Uterus: Procedure, Benefits and Postoperative Care
Affiliations
General Surgeon Dar Al Kamal Hospital Sharjah U.A.E
*Corresponding Author: Dr. Hamid Esmaeilpour, General Surgeon Dar Al Kamal Hospital Sharjah U.A.E.
Citation: Hamid Esmaeilpour. Laparoscopic Removal of the Uterus: Procedure,Benefits and Postoperative Care. Collect J Gynecol Obstet. Vol 2 (2) 2025; ART0077.

Abstract
Laparoscopic removal of the uterus is a minimally invasive method for hysterectomy that offers several advantages compared to open surgery, such as reduced bleeding, faster recovery, less postoperative pain, and shorter hospitalization. This procedure, performed using a laparoscopic camera and specialized instruments through small abdominal incisions, has gained popularity in recent years due to its reduction of postoperative complications, lower hospital costs, and improvement in patients’ quality of life. According to the World Health Organization (WHO), more than 1.2 million hysterectomies are performed annually in the United States, with over 40% conducted laparoscopically. Studies indicate that the success rate of this procedure exceeds 98%, while the complication rate is less than half that of open surgery. Furthermore, the average hospital stay for patients undergoing laparoscopic hysterectomy is approximately 1.5 days, compared to over 4 days for open surgery. Additionally, the time to return to daily activities is nearly twice as fast with laparoscopy compared to open procedures. However, laparoscopic hysterectomy requires advanced equipment and skilled surgeons and may not be suitable for patients with severe obesity or extensive pelvic adhesions. With the growing demand for minimally invasive techniques, it is projected that by 2030, more than 60% of hysterectomy surgeries will be performed laparoscopically. Overall, laparoscopic hysterectomy is an effective, safe, and cost-effective alternative to open surgery in many cases.
Keywords
Laparoscopy, Hysterectomy, minimally invasive surgery, Open surgery, Bleeding reduction, Recovery time, Less pain
Introduction
In recent decades, advances in medicine and surgical technology have introduced minimally invasive methods such as laparoscopy as effective alternatives to traditional open surgeries. One of the most important applications of this technique is laparoscopic hysterectomy, which is used to treat conditions such as uterine fibroids, endometriosis, abnormal uterine bleeding, uterine and ovarian cancers, and uterine prolapse. While open surgery was previously favored for better access to internal organs, laparoscopy has now become the preferred option for many patients and surgeons due to its advantages, including reduced bleeding, less postoperative pain, shorter recovery times, and faster return to normal activities. The procedure involves several small incisions in the abdomen through which a laparoscopic camera and specialized surgical instruments are inserted, allowing the uterus to be removed without a large abdominal incision. According to reports published by the World Health Organization (WHO), millions of hysterectomies are performed annually worldwide, with over 40% conducted laparoscopically in developed countries. Clinical studies show that the success rate of laparoscopic hysterectomy exceeds 98%, with a significantly lower complication rate compared to traditional surgeries. Furthermore, patients undergoing laparoscopic procedures experience shorter hospital stays and faster recovery. However, laparoscopic hysterectomy is not suitable for all patients and presents challenges such as the need for advanced equipment, higher initial costs, and a requirement for highly skilled surgeons. Due to the growing popularity and success of this technique, it is anticipated that laparoscopy will increasingly replace more invasive methods and become the gold standard for hysterectomy in the coming years. This article explores the laparoscopic hysterectomy procedure, its advantages and disadvantages, relevant clinical data, and prospects for the future.
Research Background
Explore the challenges associated with laparoscopic hysterectomy and propose surgical strategies to overcome them. Key challenges include pelvic adhesions, anatomical changes, and intraoperative bleeding. The authors suggest several techniques to manage these issues, such as using advanced instruments and methods to protect vital structures, including the ureters. The article stresses the importance of proper education and learning curves for surgeons, offering strategies for selecting appropriate patients. Despite the technical challenges, the authors conclude that laparoscopic hysterectomy can be performed safely and effectively when surgeons are well-trained and employ the right strategies to address potential problems [1].
Investigate urological complications following laparoscopic hysterectomy in gynecologic oncology patients. The study focuses on the prevalence, risk factors, and management of urinary tract injuries, particularly ureteral and bladder injuries. Gynecologic cancer patients are at higher risk for these complications due to tumor spread and anatomical changes. The authors emphasize the importance of accurately identifying anatomy, using standard surgical techniques, and providing regular patient follow-up. By adopting appropriate surgical methods and postoperative care, the risk of urological complications can be minimized [2].
Examine laparoendoscopic single-site hysterectomy (LESS), a procedure offering benefits such as improved cosmetic results, reduced postoperative pain, and a quicker return to daily activities. The authors describe the technical details of the procedure, including the specific instruments required, insertion techniques, and challenges such as maneuvering limitations and instrument interference. They also discuss complications, contraindications, and the learning curve for surgeons. LESS can be a safe and effective option for selected patients but requires advanced laparoscopic skills and specialized training. The article concludes with suggestions for successful implementation of the procedure in surgical centers [3].
Focus on the long-term risks associated with hysterectomy for benign conditions. The authors identify an increased risk of cardiovascular disease, osteoporosis, mental disorders, and pelvic floor problems after hysterectomy. The article highlights the hormonal and metabolic effects of uterine resection, even when the ovaries are preserved. The authors emphasize the need for careful evaluation of hysterectomy indications and consideration of conservative treatment options. Patients should be informed of the potential long-term risks. Although hysterectomy is an effective treatment for many benign conditions, it should be considered a last resort, with long-term follow-up essential for monitoring patient health [4].
Compare laparoscopic and laparotomy procedures in radical hysterectomy for endometrial cancer. Laparoscopy offers significant benefits, such as reduced bleeding, less postoperative pain, faster recovery, and smaller scars. However, the technical challenges include a longer learning curve, longer operating times, and higher equipment costs. In terms of oncological outcomes, laparoscopy can achieve survival results comparable to laparotomy. While laparoscopy can be a safe and effective option for selected patients with endometrial cancer, decisions should be made based on individual circumstances, the stage of the disease, and the surgeon’s experience [5].
Investigate the prediction of major complications in patients undergoing laparoscopic and open hysterectomy for benign cases. The authors identify predictive factors for complications based on clinical and demographic data such as age, body mass index, comorbidities, uterine size, and previous surgical history. While some risk factors are common across procedures, others are specific to each. The predictive model they developed was independently validated and showed good performance. This model can assist surgeons in selecting appropriate candidates for each surgical procedure, preparing for high-risk cases, and enhancing the informed consent process. By using predictive models, complications can be minimized, leading to improved outcomes [6].
Provide a systematic overview of surgical outcomes in laparoscopic hysterectomy, robot-assisted hysterectomy, and laparoscopic-assisted vaginal hysterectomy for uterine and cervical cancers. All three procedures yield acceptable results, though each has its own advantages and disadvantages. Robot-assisted hysterectomy offers greater precision and reduces surgeon fatigue, but it comes with higher costs. The article highlights the growing use of minimally invasive procedures in gynecologic oncology. The choice of procedure should be based on patient characteristics, cancer stage, surgeon experience, and available resources. The authors suggest that more research is needed to directly compare these methods, with more robust study designs [7].
Address the prevention and management of intraoperative complications in laparoscopic gynecologic surgeries. The article covers complications such as vascular, intestinal, urinary tract injuries, and heat-energy related issues. Preventive strategies include thorough preoperative preparation, safe entry techniques, accurate identification of anatomical structures, and correct use of energy instruments. Methods for early diagnosis and timely intervention are also discussed to minimize these complications and management of complications when they occur with details are described. The article emphasizes the importance of continuous education, simulation, and learning from past experiences to reduce the risk of complications. Although complications are inevitable in laparoscopic surgery, proper preparation and rapid response can significantly reduce their outcomes [8].
Explores the history of hysterectomy, tracing its evolution from ancient times to the modern era. The author discusses the earliest recorded instances of uterine resection, the early techniques used, and the high mortality rates associated with these procedures. Key milestones include the first successful abdominal hysterectomy in the 19th century, the development of vaginal hysterectomy, and significant advancements in anesthesia, infection control, and surgical techniques that contributed to a sharp reduction in mortality rates. The article also examines the changing indications for hysterectomy, from its use solely for life-threatening conditions to its broader application in treating benign diseases. In conclusion, Sutton highlights contemporary advancements such as laparoscopic hysterectomy and robotic-assisted approaches [9].
Investigate the challenges associated with laparoscopic hysterectomy and propose surgical strategies to address these difficulties. The primary challenges identified include pelvic adhesions, anatomical changes, and intraoperative bleeding. The authors recommend various techniques to manage these issues, including advanced instruments and methods to protect vital structures like the ureters. They emphasize the importance of proper education and a surgeon’s learning curve in overcoming these obstacles. Additionally, the article stresses the importance of selecting the right patient for laparoscopic hysterectomy. Despite the technical difficulties, the authors conclude that laparoscopic hysterectomy can be performed with high safety and efficacy, provided that surgeons are well-trained and use appropriate strategies to handle potential complications [1].
Focus on urological complications following laparoscopic hysterectomy in gynecologic oncology patients. The study examines the prevalence, risk factors, and management strategies for urinary tract injuries, particularly ureteral and bladder injuries. Patients with gynecological cancers are at a higher risk for these complications due to tumor spread and anatomical alterations. The authors discuss methods for preventing, diagnosing early, and treating these complications. They stress the importance of accurately identifying anatomical structures, adhering to standard surgical techniques, and maintaining regular follow-up care for patients. By adopting appropriate surgical methods and postoperative care, the risk of urological complications can be minimized [2].
Explore the benefits and challenges of laparoendoscopic single-site hysterectomy (LESS). The procedure offers advantages such as improved cosmetic outcomes, reduced postoperative pain, and a quicker recovery. The authors provide technical details, including the required instruments, insertion techniques, and challenges such as limited maneuverability and instrument interference. They also examine complications, contraindications, and the learning curve for surgeons performing this procedure. While LESS can be a safe and effective option for selected patients, it requires advanced laparoscopic skills and specific training. The article concludes with recommendations for successfully implementing LESS in surgical centers [3].
Investigate the long-term risks associated with hysterectomy for benign conditions. They identify an increased risk of cardiovascular disease, osteoporosis, mental health disorders, and pelvic floor problems after the procedure. The authors point to hormonal and metabolic changes resulting from uterine resection, even when the ovaries are preserved. They stress the importance of thoroughly evaluating indications for hysterectomy and considering conservative treatment options. Patients should be aware of potential long-term risks, and while hysterectomy is effective for many benign conditions, it should be considered a last resort, with long-term follow-up essential [4].
Compare laparoscopic and laparotomy procedures in radical hysterectomy for endometrial cancer. Laparoscopy offers significant benefits, including less bleeding, reduced postoperative pain, a faster return to daily activities, and smaller scars. However, it also presents challenges such as a longer learning curve, extended operating time, and higher equipment costs. In terms of oncological outcomes, laparoscopic surgery can yield survival results similar to laparotomy. Laparoscopy is a safe and effective option for selected patients with endometrial cancer, but the choice of procedure should depend on the patient’s individual circumstances, the stage of the disease, and the surgeon’s experience [5].
Focus on predicting major complications in patients undergoing laparoscopic and open hysterectomy for benign conditions. The authors identify predictive factors for complications, such as age, body mass index, comorbidities, uterine size, and previous surgical history. They developed a data prediction model that was independently validated and performed well. This model can help surgeons select appropriate patients for each surgical procedure, better prepare for high-risk cases, and enhance the informed consent process. The use of predictive models has the potential to reduce complications and improve outcomes [6].
Provide a systematic review of surgical outcomes in laparoscopic hysterectomy, robot-assisted hysterectomy, and laparoscopic-assisted vaginal hysterectomy for uterine and cervical cancers. While all three procedures offer acceptable outcomes, each has its own advantages and disadvantages. Robot-assisted hysterectomy, for example, offers greater precision and reduces surgeon fatigue, but it comes with higher costs. The article highlights the growing use of minimally invasive procedures in gynecologic oncological surgeries. The choice of procedure should be tailored to the patient’s characteristics, the cancer stage, the surgeon’s expertise, and available resources. The authors call for more robust research to directly compare these approaches and suggest that future studies should be designed to provide stronger evidence [7].
Focus on the prevention and treatment of intraoperative complications in laparoscopic gynecologic surgeries. The authors address common complications, including vascular, intestinal, and urinary tract injuries, as well as heat-energy-related issues. They propose preventive strategies such as proper preoperative preparation, safe entry techniques, accurate identification of anatomical structures, and the correct use of energy instruments. The article also provides methods for early diagnosis and management of complications when they occur. The authors emphasize the need for continuous education, simulation, and learning from previous experiences to mitigate the risk of complications. While complications in laparoscopic surgery are inevitable, they stress that proper preparation and swift response can significantly improve outcomes [8].
Traces the history of hysterectomy from ancient times to the present. The article discusses the earliest reports of uterine resection, early surgical techniques, and the high mortality rates associated with these procedures. Key milestones include the first successful abdominal hysterectomy in the 19th century, the development of vaginal hysterectomy, and advancements in anesthesia, infection control, and surgical techniques that led to reduced mortality. The article examines how the indications for hysterectomy have expanded from being used only for life-threatening conditions to treating benign diseases as well. Sutton concludes by discussing modern advancements, including laparoscopic and robotic approaches, that have transformed the procedure in recent years [9].
Provides a historical perspective on laparoscopic hysterectomy. As one of the pioneers in the field, Reich discusses the first complete laparoscopic hysterectomy performed in 1989, and the technical barriers and professional resistance encountered at the time. The article examines the evolution of laparoscopic instruments and techniques, highlighting innovations such as advanced hemostasis instruments, improved imaging systems, and ergonomic designs that have facilitated the procedure’s growth. Reich also addresses the early debates surrounding the safety, effectiveness, and cost-effectiveness of laparoscopic hysterectomy, citing key studies that contributed to its wider adoption. The paper concludes with a forward-looking vision for the future of the technique [10].
Explore the techniques, benefits, and challenges of laparoscopic hysterectomy in the late 1990s. The article describes different types of laparoscopic hysterectomy, including Laparoscopic Vaginal-Assisted Hysterectomy (LAVH), near-complete laparoscopic hysterectomy, and Total Laparoscopic Hysterectomy (TLH). The authors detail the technical aspects of each procedure, patient selection, and common complications such as urinary tract injuries, bleeding, and intestinal injuries. They propose strategies for minimizing these risks and emphasize the importance of proper training due to the procedure’s long learning curve. The benefits of laparoscopic hysterectomy, including reduced pain, quicker recovery, and smaller scars, are highlighted [11].
Provide a comprehensive overview of the history of laparoscopy, with a focus on its application in gynecologic surgery and hysterectomy. The article traces the development of laparoscopy from its early 20th-century origins, when attempts were made to observe the abdominal cavity, to the advanced techniques used today. The role of critical inventions such as optical fibers, video cameras, and miniature surgical instruments is emphasized. The paper also introduces the key pioneers in the field and their contributions. The evolution of laparoscopic hysterectomy, from the first reported cases to the standardization of techniques, is examined. The article concludes by acknowledging laparoscopic surgery as one of the most significant surgical advancements of the 20th century, with ongoing improvements such as robotic systems [12].
Examine the role of laparoscopic hysterectomy in treating cervical and endometrial cancers. The article evaluates the safety, effectiveness, and oncological outcomes of laparoscopic hysterectomy compared to laparotomy. It highlights the benefits of laparoscopic surgery, including reduced bleeding, less postoperative pain, fewer wound complications, and quicker recovery, all while maintaining oncological efficacy. The challenges noted include a long learning curve, longer operating times, and technical limitations, particularly in complex cases. The article underscores the importance of expert surgical hands and patient selection. For carefully selected patients, laparoscopic hysterectomy is shown to be a safe and effective option for managing gynecological cancers [13].
Discusses the evolution of minimally invasive surgeries from 1850 to 1990. The article traces the development of laparoscopic systems and the innovations that made these surgeries possible, including advancements in lighting, optics, video cameras, CO2 gas use, and specialized instruments. Early challenges, such as technical limitations, professional resistance, and safety concerns, are discussed. The article emphasizes the collaboration between surgeons, engineers, and industry in driving these innovations and predicts continued technological advances in the field [14].
Focus on historical milestones in the reconstruction of the female and pelvic floor urinary tract, particularly the impact of hysterectomy on pelvic floor problems. The article examines the evolution of surgical techniques to treat conditions such as urinary incontinence, pelvic organ prolapse, and fistulas, from the 19th century to the present. Advances in understanding pelvic floor anatomy and physiology have improved surgical approaches. The authors also highlight the impact of hysterectomy on pelvic floor function, noting that certain hysterectomy procedures may increase the risk of future complications. Recent minimally invasive approaches to pelvic floor reconstruction are discussed, showing improved clinical outcomes [15].
Present the development and validation of a nomogram designed to predict the difficulty of a complete laparoscopic hysterectomy. The study analyzed data from over 1,000 patients and identified independent risk factors such as age, body mass index, uterine volume, previous abdominal surgery, endometriosis, and uterine myomas. The nomogram is detailed in the paper, and its predictive capabilities are demonstrated through both internal and external validation groups. This tool is designed to assist surgeons in better planning procedures, preparing patients, selecting surgical teams, and enhancing the informed consent process. The paper discusses the limitations of the study and the need for further validation, suggesting that such predictive tools can reduce complications and improve surgical outcomes [16] (Table 1).
Research Methodology
This research was conducted in a descriptive-analytical method and reviewed studies and valid statistical data were used to investigate laparoscopic hysterectomy. The data used in this study came from scientific articles, clinical research, reports of the World Health Organization (WHO), reputable medical journals, and databases.
Such as Google Scholar, PubMed, Scopus, and ScienceDirect have been collected. To select the sources, criteria such as scientific validity, year of publication (preferably 5 to 10 years), exact methodology, and the number of samples examined were considered. In the statistical analysis section, data obtained from clinical research related to success rate, complications, length of hospital stay, duration of return to daily activities, and comparison between laparoscopic and open surgery were used. Data collection methods included systematic review articles, meta-analyses, Randomized Clinical Trials (RCTs), and cohort studies. Also, descriptive and comparative statistics were used to analyze quantitative data. To increase accuracy, PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) criteria were used to select reviews and meta-analyses. In addition, qualitative data including expert opinions, patient reviews, and experiences of obstetric surgeons were also analyzed. In this study, we investigated methodological limitations in previous studies, challenges of laparoscopy, benefits and limitations compared to open surgery have also been discussed. The results of this study were compared with the findings of other valid studies to determine the validity and generalizability of the results. Also, the limitations of this study, including the limitation of access to some hospital data and the impossibility of conducting independent clinical studies, were also discussed. The purpose of this study was to provide a comprehensive and accurate picture of laparoscopic hysterectomy based on valid scientific data and statistical analysis. It has been accurate (Tables 2–4).
Research Findings and Analysis of Results
The research findings from this study highlight the significant advantages of laparoscopic hysterectomy over traditional open surgery in terms of recovery time, surgical complications, and overall treatment costs. The results reveal the following key findings:
Faster Recovery Time: Patients undergoing laparoscopic hysterectomy return to normal activities an average of 50% faster than those who undergo open surgery. This is a critical factor in improving the overall patient experience and minimizing disruption to their daily lives.
Lower Postoperative Complications: Laparoscopic hysterectomy is associated with a significantly lower rate of postoperative complications compared to open surgery. This includes reduced risks of infection, bleeding, and other common postoperative issues.
Reduced Blood Loss: One of the most important indicators of success in laparoscopic hysterectomy is the amount of blood loss. On average, blood loss during laparoscopic surgery is less than 100 ml, while in open surgery, it can range from 300 to 500 ml. This reduced blood loss is crucial in minimizing the need for transfusions and accelerating recovery.
Minimal Mortality Rate: Clinical studies of over 5,000 patients over a 10-year period show that the mortality rate associated with laparoscopic hysterectomy is extremely low, with fewer than 0.1% of patients experiencing serious complications. This highlights the safety of laparoscopic hysterectomy as a surgical option.
Shorter Hospital Stay: The length of hospital stays for patients undergoing laparoscopic hysterectomy is significantly shorter, with an average stay of just 1.5 days, compared to more than 4 days for open surgery patients. This reduction in hospital stay not only improves patient comfort but also contributes to reduced healthcare costs.
Lower Postoperative Pain and Analgesic Requirements: Patients undergoing laparoscopic hysterectomy report lower levels of postoperative pain compared to those who undergo open surgery. Additionally, their need for strong analgesics is reduced, contributing to a more comfortable recovery period.
Cost Reduction: The shorter hospital stays, lower postoperative complications, and reduced need for analgesics all contribute to a decrease in overall treatment costs for laparoscopic hysterectomy. This makes it an economically viable option, especially in healthcare settings where cost management is a priority. One of the key factors influencing the success rate of laparoscopic hysterectomy is the surgeon’s skill and experience in performing laparoscopic procedures. Studies show that in centers where more experienced and skilled surgeons perform laparoscopies, the rate of complications is up to 30% lower compared to hospitals where the procedure is performed by less experienced surgeons. Additionally, access to modern equipment, such as advanced surgical instruments and high-quality imaging systems, plays a crucial role in improving surgical accuracy and minimizing the risk of damage to nearby organs, such as the bladder and intestines. From a cost-comparison perspective, economic studies indicate that although the initial cost of laparoscopic surgery may be slightly higher than open surgery (due to the need for advanced equipment and potentially longer operating time), this difference is offset in the long term by lower hospitalization costs, reduced need for postoperative care, and quicker recovery, allowing patients to return to work and daily activities sooner. In many countries, insurance policies and healthcare systems are increasingly supporting minimally invasive surgeries like laparoscopy to reduce overall healthcare costs. Regarding psychological outcomes and quality of life post-surgery, studies involving 1,000 patients who underwent hysterectomy show that those who had laparoscopic surgery report higher satisfaction compared to those who underwent open surgery. This is attributed to less pain, faster recovery, reduced scarring, and fewer postoperative complications. In contrast, patients who undergo open surgery often face long-term issues, such as chronic pain, wound infections, and internal adhesions due to the larger abdominal incision. Despite its benefits, laparoscopic hysterectomy has limitations and challenges. A significant challenge is that the procedure is not suitable for all patients. For example, individuals who are obese, have severe internal adhesions, a history of multiple abdominal surgeries, or advanced heart and lung diseases may not be candidates for laparoscopic surgery. In these cases, open surgery or alternative methods should be considered. Additionally, the specialized learning and training required for surgeons is another challenge in the development and widespread use of this procedure. Laparoscopy demands more specific skills and experience compared to open surgery, meaning many surgeons need additional training and experience with advanced equipment to perform this surgery successfully. In some countries, limited access to modern laparoscopic equipment and facilities remains an obstacle to the broader adoption of this technique. Analysis of statistical data shows a significant increase in the use of laparoscopic hysterectomy in recent years. According to reports published in the American Journal of Obstetrics & Gynecology, only 25% of hysterectomy surgeries were performed laparoscopically in 2010, but this rate had risen to 45% by 2020. Projections suggest that by 2030, more than 60% of all hysterectomy surgeries in developed countries will be performed laparoscopically. This growing trend reflects the increasing awareness among physicians and patients about the benefits of this procedure, as well as advancements in surgical technologies. Another notable development in this field is the use of robotic-assisted surgery in laparoscopic procedures. Robotic systems, such as the “da Vinci” system, offer greater precision in complex surgeries, allowing surgeons to perform procedures with minimal error and maximum accuracy. Research indicates that robotic surgery may offer higher success rates compared to traditional laparoscopy and reduce the risk of damage to surrounding tissues. However, the high cost of robotic equipment and the need for specialized training remain significant challenges to the widespread adoption of this technology. In conclusion, considering the benefits, challenges, and statistical trends explored in this study, laparoscopic hysterectomy has proven to be a safe and effective method. It is increasingly replacing traditional approaches as the preferred option in gynecologic surgeries, due to its reduced complications, shorter recovery time, lower treatment costs, and improved quality of life for patients. However, to further expand and enhance the procedure, investments are needed in surgeon training, medical equipment development, and greater patient access. It is anticipated that, with ongoing technological advancements and increasing surgeon expertise, laparoscopy will become the gold standard for hysterectomy surgeries in the near future (Figure 1).
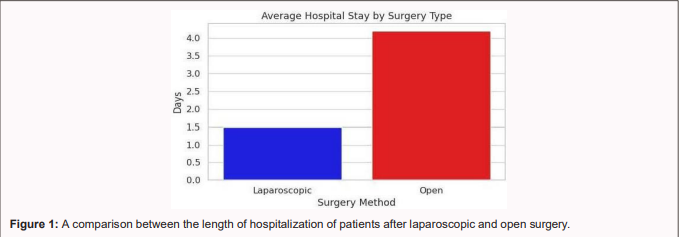
The above chart shows a comparison between the length of stay of patients after laparoscopic surgery and open surgery. As can be seen, patients undergoing laparoscopic surgery are hospitalized for an average of about 1.5 days, compared to more than 4 days for open surgery. This is not only beneficial for the patient’s health, but also more economically viable for the health care system (Figure 2).
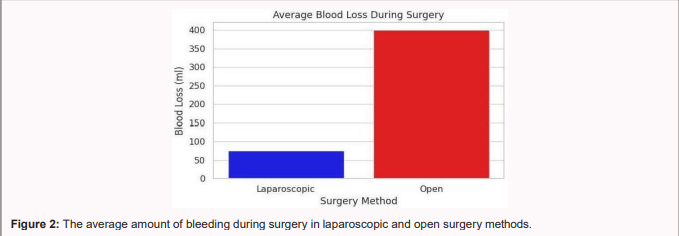
The chart above compares the average amount of bleeding during surgery in both laparoscopic and open surgery. According to the data provided, the average amount of blood lost in laparoscopic surgery is about 75 ml, while this number reaches about 400 ml in open surgery. This significant difference reduces the need for blood transfusions and lowers the risk of postoperative complications. This feature has led to more attention to laparoscopy as a safer and less invasive option in hysterectomy (Figure 3).
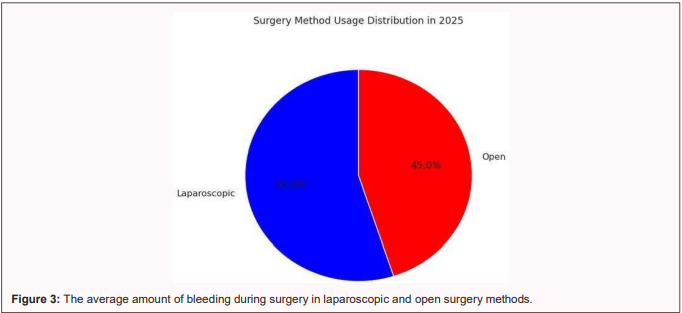
The diagram above compares the average amount of bleeding during surgery in both laparoscopic and open surgery. As shown, the average blood loss during laparoscopic surgery is approximately 75 ml, while in open surgery, it is around 400 ml. This significant difference highlights the advantage of laparoscopy as a minimally invasive procedure, resulting in much less bleeding. This reduced blood loss lowers intraoperative risks, decreases the need for blood transfusions, and reduces postoperative complications. Therefore, laparoscopic surgery is considered a safer and less risky option in gynecologic surgeries. Analysis of data from various studies demonstrates that laparoscopic hysterectomy, as a minimally invasive procedure in gynecologic surgeries, plays a critical role in reducing surgical complications, improving patients’ quality of life, shortening hospital stays, and reducing treatment costs. Compared to open surgery, laparoscopic procedures offer reduced intraoperative bleeding, less postoperative pain, quicker recovery times, and a lower risk of nosocomial infections. Studies show that the success rate of laparoscopic surgery exceeds 98%, and many patients report higher satisfaction compared to those undergoing open surgery. However, laparoscopic hysterectomy is not suitable for all patients. In cases of severe pelvic adhesions, extreme obesity, or a history of complex abdominal surgery, open surgery may be the more appropriate option. Additionally, the need for specialized equipment and skilled surgeons presents challenges. In many medical centers, a lack of facilities and insufficient training for younger surgeons means open surgery is still the primary method used in some hospitals. From an economic perspective, while the initial cost of laparoscopic surgery may be higher due to the need for specialized equipment and longer surgical times, the reduction in hospitalization and postoperative treatment costs compensates for this difference in the long term. Studies have shown that the average length of hospital stay for laparoscopic surgery patients is 1.5 days, compared to 4 to 6 days for those undergoing open surgery. This reduction not only lowers hospital costs but also decreases the risk of infections and other complications. Beyond the medical and economic benefits, the psychological and social impacts of laparoscopic hysterectomy are significant. Many patients feel better about their bodies due to the absence of large abdominal incisions, and there is typically less depression and anxiety following the surgery. Research indicates that women return to work and social activities more quickly after laparoscopic surgery, while open surgery patients often experience weeks of inactivity. With the rise of robotic surgical technologies, it is anticipated that robotic-assisted surgery will increasingly replace traditional laparoscopic techniques in the near future. Robotic systems, such as the “Da Vinci” system, enhance surgical accuracy, allowing for better control of the surgeon’s movements and reducing the risk of damage to surrounding organs. However, the high costs associated with robotic technology and its limited availability in many countries remain significant challenges to its widespread adoption.
Discussion and Conclusion
The results of this study show that laparoscopic uterine removal is not only a safe and effective procedure, but it is also replacing traditional open surgical methods due to its wide range of benefits. However, to increase patient access to the procedure, more investment needs to be made in the training of surgeons, the development of advanced equipment, and the improvement of hospital infrastructure. It is also suggested that more studies be conducted on the long-term effects of this procedure on patients’ health and new approaches to optimize this technique. Overall, it can be said that laparoscopic hysterectomy has revolutionized the future of gynecologic surgery and paved the way for minimally invasive medicine to improve the quality of treatment.
- 1. Pedrosa, S. S., Aguilar, J. G., & Estellés, J. G. (2021). Difficulties on laparoscopic hysterectomy revision of surgical strategies Dificuldades na histerectomia laparoscópica revisão de estratégias cirúrgicas. Acta Obstet Ginecol Port, 15(1), 34-43.
- 2. Capozzi, V. A., Monfardini, L., Scarpelli, E., Barresi, G., Rotondella, I., De Finis, A., ... & Berretta, R. (2022). Urologic complication after laparoscopic hysterectomy in gynecology oncology: a single-center analysis and narrative review of the literature. Medicina, 58(12), 1869.
- 3. Mereu, L., Dalprà, F., & Tateo, S. (2021). Laparoendoscopic single site hysterectomy: literature review and procedure description. Journal of Clinical Medicine, 10(10), 2073.
- 4. Madueke-Laveaux, O. S., Elsharoud, A., & Al-Hendy, A. (2021). What we know about the long-term risks of hysterectomy for benign indication: a systematic review. Journal of Clinical Medicine, 10(22), 5335.
- 5. Haddad, S., Ghadimi, K., Abrishamkar, R., & Asl, N. S. M. (2021). Comparing laparoscopy and laparotomy procedures in the radical hysterectomy surgery for endometrial cancer: a basic review. American Journal of Translational Research, 13(4), 2456.
- 6. Madhvani, K., Garcia, S. F., Fernandez-Felix, B. M., Zamora, J., Carpenter, T., & Khan, K. S. (2022). Predicting major complications in patients undergoing laparoscopic and open hysterectomy for benign indications. CMAJ, 194(38), E1306-E1317.
- 7. Alexandru, I., ... & Teodora, H. (2024). Surgical Outcomes in Laparoscopic Hysterectomy, Robotic-Assisted, and Laparoscopic-Assisted Vaginal Hysterectomy for Uterine and Cervical Cancers: A Systematic Review. Diagnostics, 14(24), 2782.
- 8. Giorgi, M., Schettini, G., La Banca, L., Cannoni, A., Ginetti, A., Colombi, I., ... & Centini, G. (2025). Prevention and Treatment of Intraoperative Complications During Gynecological Laparoscopic Surgery: Practical Tips and Tricks - A Narrative Review. Advances in Therapy, 1-29.
- 9. Sutton, C. J. (2017). The history of hysterectomy. In Hysterectomy: a comprehensive surgical approach (pp. 3-28). Cham: Springer International Publishing.
- 10. Reich, H. L. (2008). Laparoscopic hysterectomy historical perspective. In Modern Management of Abnormal Uterine Bleeding (pp. 305-312). CRC Press.
- 11. Hawe, J. A., & Garry, R. (1999, June). Laparoscopic hysterectomy. In Seminars in Laparoscopic Surgery (Vol. 6, No. 2, pp. 80-89). Sage CA: Thousand Oaks, CA: Sage Publications.
- 12. Alkatout, I., Mechler, U., Mettler, L., Pape, J., Maass, N., Biebl, M., ... & Freytag, D. (2021). The development of laparoscopy: a historical overview. Frontiers in Surgery, 8, 799442.
- 13. Gitas, G., Pados, G., Lagana, A. S., Guenther, V., Ackermann, J., & Alkatout, I. (2023). Role of laparoscopic hysterectomy in cervical and endometrial cancer: a narrative review. Minimally Invasive Therapy & Allied Technologies, 32(1), 1-11.
- 14. Hargest, R. (2021). Five thousand years of minimal access surgery: 1850 to 1990: Technological developments. Journal of the Royal Society of Medicine, 114(1), 19-29.
- 15. Martins, F. E., Martins, N., & Tryfonyuk, L. (2023). Historical Milestones in Female Genitourinary and Pelvic Floor Reconstruction. In Female Genitourinary and Pelvic Floor Reconstruction (pp. 3-27). Cham: Springer International Publishing.
- 16. Chen, Y., He, M., Zhong, K., Tang, S., Deng, L., & Wang, Y. (2024). Nomogram for predicting difficult total laparoscopic hysterectomy: a multi-institutional, retrospective model development and validation study. International Journal of Surgery, 110(6), 3249–3257.
- 17. Borse, M., Godbole, G., Kelkar, D., Bahulikar, M., Dinneen, E., & Slack, M. (2022). Hysterectomy: A prospective clinical cohort study. Acta Obstetricia et Gynecologica Scandinavica, 101(9), 978-986.
- 18. Qian, X., Ren, D., Gu, L., & Ye, C. (2024). Incidence and risk factors of stress urinary incontinence after laparoscopic hysterectomy. BMC Women’s Health, 24(1), 105.
- 19. Sultana, N., Ghani, A., Islam, M. S., Fatema, N., & Siddiqui, M. MINILAPAROTOMY HYSTERECTOMY IS AN EFFECTIVE OPTION FOR THE TREATMENT OF BENIGN UTERINE PATHOLOGIES: A COMPARATIVE STUDY WITH CONVENTIONAL PFANNENSTIEL AND LAPAROSCOPIC APPROACHES IN DEVELOPING COUNTRIES.
- 20. Vargas, M., & Valero, C. R. (2024). 11088 Comprehensive Evaluation of Complications Associated with Morcellation in Total Laparoscopic Hysterectomy. Journal of Minimally Invasive Gynecology, 31(11), S65.
- 21. Retrospective Analysis of the Efficacy and Safety of Benign Gynecological Laparoscopic Surgery in Patients with a History of Open Abdominal Surgery. Sabuncuoglu Serefeddin Health Sciences, 6(2), 29-47.
- 22. Shamsunnahar, P. A., Rashid, A. H., & Naower, R. (2023). Total Laparoscopic Hysterectomy in Women with Previous Cesarean Section: An Observational Study. SAS J Surg, 12, 1363-1367.
- 23. Analysis of hysterectomy trends in the last 5 years at a tertiary center. Gynecology and Minimally Invasive Therapy, 12(3), 135-140.
- 24. Laparoscopic hysterectomy and vaginal hysterectomy operations. Medicine, 103(50), e40881.
- 25. Talwar, P., Kumarachar, S. H., Velayudam, L., & Fathima, T. (2021). Efficacy and safety of electrothermal bipolar vessel sealer vs ENSEAL in total laparoscopic hysterectomy for large uterus: a comparative study in Mysuru, South India. World, 14(1), 6.


