- 1. Al-Akchar M, Shams P, Kiel J: Acute Myocarditis. [Updated 2023 Jul 5]. In. StatPearls [Internet, Treasure Island (FL): StatPearls Publishing; 2023.
- 2. Caforio AL, Pankuweit S, Arbustini E, et al.: Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013, 34:2636-48. 10.1093/eurheartj/eht210
- 3. Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013, 34:2636-48. 10.1093/eurheartj/eht210
- 4. Ammirati E, Moslehi JJ: Diagnosis and Treatment of Acute Myocarditis: A Review. JAMA. 2023, 4:1098- 1113. 10.1001/jama.2023.3371
- 5. Narula, J., Khaw, B. A., & Dec, G. W. (1993): Recognition of acute myocarditis masquerading as acute myocardial infarction. New England Journal of Medicine. 328:100-104.
- 6. Wang, K., Asinger, R. W., & Marriott, H. J. (2003): ST-Segment elevation in conditions other than acute myocardial infarction. The New England Journal of Medicine. 349:2128-2135.
- 7. Costantini M, Oreto G, Albanese A, et al.: Presumptive myocarditis with ST-Elevation myocardial infarction presentation in young males as a new syndrome. Clinical significance and long-term follow-up. Cardiovasc Ultrasound 9, 1 . . 2011. 10.1186/1476-7120-9-1
- 8. Buttà C, Zappia L, Laterra G, et al.: Diagnostic and prognostic role of electrocardiogram in acute myocarditis: A comprehensive review. Ann Noninvasive Electrocardiol. 2020, 25:12726. 10.1111/anec.12726
- 9. Friedrich MG, Sechtem U, Schulz-Menger J, et al.: International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis. JACC White Paper. J Am Coll Cardiol. 2009, 8:1475-87. 10.1016/j.jacc.2009.02.007.
Journal Menu
Articles
Useful links
- Peer Review
- Why Submit?
- Submission Checklist
- Article Types
- Instructions for Authors
- Article Processing Fee
Home Menu
Affiliations *Corresponding Author:
Majed Sheikh, Cardiology, Royal Free London Foundation Trust, London, GBR
Citation:
Sheikh M, Ioakim K, Besis G, Masri A, Gopalakrishnan PP. Title CMR Importance in Diagnosing Myocarditis Presenting as Inferolateral STEMI Institutions.
Collect J Cardiovasc Med. Vol 2 (1) 2025; ART0073.
We present a case of a 20-year-old male patient who presented as an
ST-segment elevation myocardial infarction picture with typical
ECG and troponin rise, only to be found
to have normal epicardial coronary arteries on coronary angiogram. However, a
Cardiac Magnetic Resonance Imaging (CMR) was diagnostic of myocarditis.
Myocarditis is a condition characterized by inflammation of the myocardium,
typically manifesting suddenly. It is primarily attributed to viral infections like
influenza and coronavirus, autoimmune disorders such as
lupus, and certain medications like immune-checkpoint inhibitors [1].
The most prevalent symptom among patients is chest pain, although others
may experience shortness of breath or sudden fainting episodes [2].
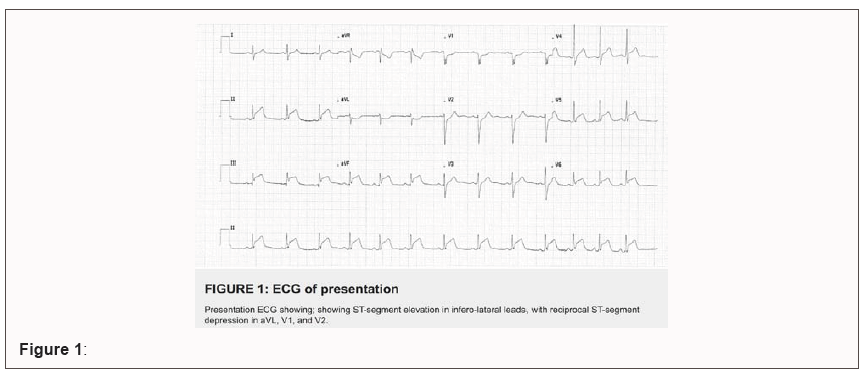
Electrocardiogram (ECG) findings in myocarditis cases are often diverse,
lacking distinctive features for definitive diagnosis [3]. Nevertheless, as
exemplified in our case, myocarditis can occasionally present with ECG alterations that strongly resemble
those seen in acute myocardial infarction, featuring ST-segment elevation.
This situation necessitates prompt evaluation through emergent coronary angiography to rule out any
coronary artery involvement. Certain demographic and clinical features can be suggestive. After ruling
out acute coronary syndromes, CMR imaging may confirm the diagnosis of myocarditis.
A 20-year-old Brazilian male was admitted to the hospital due to
chest pain. He had reported experiencing mild chest discomfort,
aggravated when lying supine, along with headaches, fevers, and joint pains
that did not respond to simple analgesia. The patient had no significant past medical history or
family history of relevant diseases. He had no personal and family medical history of note, and he had
received both doses of Coronavirus Disease 2019 (COVID-19) vaccination,
with the last dose administered one year ago. He denied any recent gastrointestinal, respiratory, or
flu-like symptoms, and had not traveled in the last three years since relocating to the United Kingdom.
Upon presentation, his ECG revealed
inferolateral ST-segment elevation coupled with an increase in
cardiac troponin (cTnT) levels (462ng/L) (Figure 1).
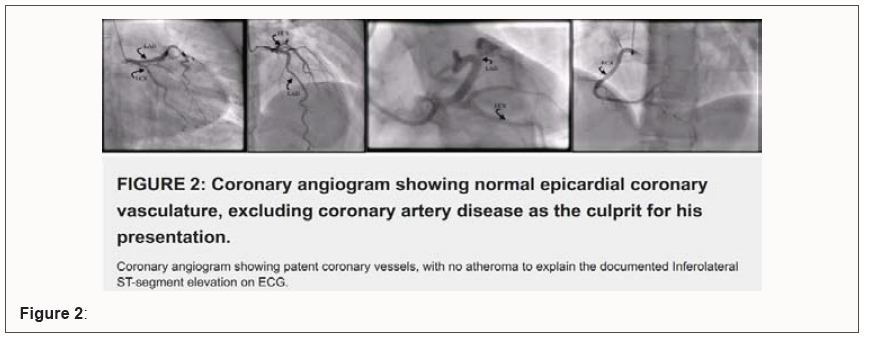
However, the coronary angiogram exhibited unobstructed coronary arteries
(Figure 2). Subsequent
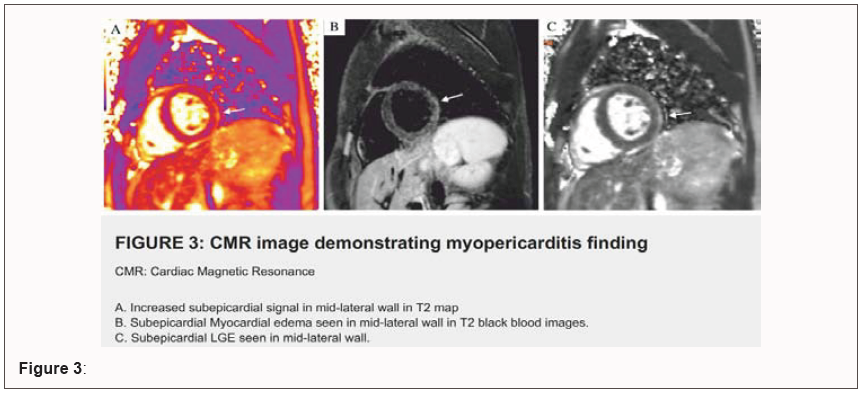
Cardiac Magnetic Resonance Imaging (CMR) performed two days later
revealed signs consistent with localized myocarditis, including increased subepicardial signal in mid-lateral
wall in T2 mapping (Figure 3A),
subepicardial myocardial edema seen in mid-lateral wall in
T2 black blood images (Figure 3B),
and subepicardial LGE (Late Gadolinium Enhancement) seen in mid-lateral
wall (Figure 3C).
Chest X-ray was unremarkable and a comprehensive myocarditis panel, as detailed below. The patient was
admitted to the hospital for cardiac rhythm monitoring and was treated with
colchicine and ibuprofen, with gradual improvement. He was then discharged
on colchicine for a period of 3 months. On follow-up, the patient had
no further symptoms and had completed his course of colchicine. A repeat
Transthoracic Echocardiogram (TTE) showed normal function.
Myocarditis is a challenging clinical entity to diagnose due to its diverse clinical presentations, which can
mimic various cardiac conditions [4,5]. In this case, the patient presented with chest pain, cTnT elevation,
and inferolateral ST-segment elevation on the ECG, a constellation of symptoms that can closely resemble a
geographic ST-Elevation Myocardial Infarction (STEMI). However, it is crucial to emphasize that an angiogram
remains an important step in the diagnostic workup to rule out unstable coronary artery disease before employing
CMR to detect myocarditis. Myocarditis is known to occasionally present with variable ST segment changes [6].
Diagnosis can be suggested by a young age, absence of Coronary Artery Disease (CAD) risk factors, preceding
viral symptoms, and diffuse ECG changes; however, as we demonstrated here, none of those features were
diagnostic in our case, which required CMR to establish the diagnosis. Patients with myocarditis can exhibit
clinical features such as chest pain, elevated troponin levels, and ECG changes that resemble those seen in STEMI.
This similarity in presentation can pose a diagnostic challenge, making it imperative to consider both conditions
during the evaluation of such patients [7]. In this case, it was imperative to perform coronary angiography to
exclude obstructive coronary artery disease. This step is crucial because timely intervention is critical in cases of acute coronary syndromes. Myocardial infarction due to coronary artery disease requires prompt revascularization,
whereas myocarditis does not. Once angiography confirmed the absence of obstructive coronary lesions, CMR
played a pivotal role in establishing the diagnosis of myopericarditis. CMR offers a non-invasive and highly
sensitive method for assessing cardiac inflammation and detecting myocardial involvement [8]. In this case, CMR
revealed evidence of acute myopericarditis with preserved biventricular systolic function, providing valuable
insights into the underlying pathological process.
In summary, myocarditis can indeed masquerade as a STEMI, emphasizing the importance of a comprehensive
diagnostic approach that includes coronary angiography to rule out coronary artery disease. Following
the exclusion of obstructive coronary lesions, CMR becomes a valuable tool for confirming the diagnosis of
myopericarditis. This case highlights the need for a meticulous and stepwise evaluation to differentiate between
these two potentially life-threatening conditions and underscores the significance of using angiography before
employing CMR in such cases.
Dr Ruta Virsinskaite, Cardiology CMR Registrar, Royal Free London Foundation Trust, London, UK.
Dr Kotecha Tushar, Interventional Cardiologist, Royal Free London Foundation Trust, London, UK.
Dr Sheref Zaghloul, Senior Cardiology Clinical Fellow, Royal Free London Foundation Trust, London, UK.
CMR Importance in Diagnosing Myocarditis Presenting as Inferolateral STEMI
1Cardiology, Royal Free London Foundation Trust, London, GBR
2Cardiology, Aultman Hospital, Canton, Ohio, USA

Abstract
Introduction
Case Presentation
Test Group / Result
Details of Test Group
Viral Screen was negative for:
COVID-19 SARS, CoV-2 RNA, Influenza A and B RNA, Hepatitis B virus surface Ag screen,
Hepatitis C virus Ab screen, HIV 1 and 2 Ab level, Parvovirus B19 IgG screen,
Parvovirus B19 IgM screen, Adenovirus DNA, CMV DNA, EBV DNA, HHV6, HHV8, and Enterovirus.
Bacteriology Interpretation was negative for:
Blood and feces cultures. This included tests for Campylobacter, Salmonella, Shigella,
E. coli, Giardia, Cryptosporidium, and INF-gamma assay.
Immunological Screen was negative for:
Cryoglobulin, anti-nuclear antibodies (ANA), Anti-centromere Ab, Anti-Ro/anti-La Ab,
La Ab, Anti-RNP Ab, Anti-Sm Ab, Anti-Sc1-70 Ab, Anti-neutrophil cytoplasmic Ab (ANCA Ab),
Anti-Jo1 Ab, complement C3, Zinc transporter 8 Ab, Islet Agn-2 Abs, and Glutamic acid decarboxylase Ab.
Discussion
Conclusions
Acknowledgements
References


