Journal Menu
Articles
Useful links
- Peer Review
- Why Submit?
- Submission Checklist
- Article Types
- Instructions for Authors
- Article Processing Fee
Home Menu
Affiliations *Corresponding Author:
Fatima Adamu, Certified Hand Therapist Rothman Orthopedic Institute Philadelphia, PA.
Citation:
Adamu F, Strohl AB, Getz C. An
Interdisciplinary Approach in the Rehabilitation of a Triple Diagnosis of Brachial Plexopathy, Thoracic Outlet Syndrome and Adhesive Capsulitis. Collect J Surg. Vol 2 (1) 2025; ART0062.
Background: A patient who sustained a rotator cuff tear while shoveling snow, developed
neurological and musculoskeletal complications post-rotator cuff repair. She was subsequently
referred to hand therapy.
Methods: Clinical evaluation, targeted therapeutic exercise instruction, collaborative problem
solving with the patient and surgical team, surgical intervention and extensive manual therapy
occurred over the course of 11 months. During hand therapy treatment, the patient also underwent
radial tunnel release and arthroscopic lysis and debridement of the glenohumeral capsule.
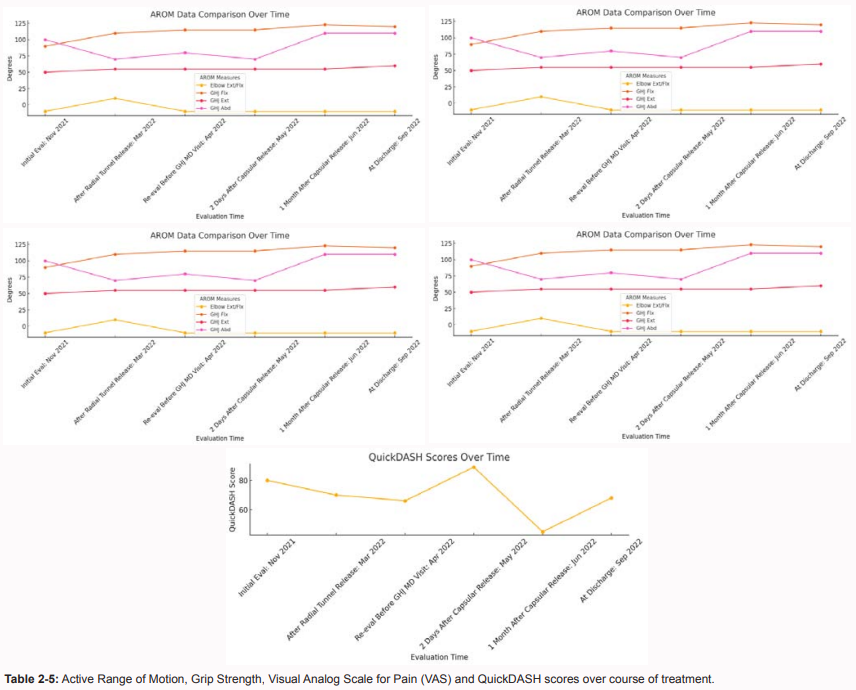
Results: Per subjective report the patient was experiencing less pain during ADLS and IADLs by
discharge. Objective measures indicate increased active and passive range of motion, overall strength
including improved grip strength, active flexion and extension at the wrist, fingers and shoulder, as
well as reduced nerve symptoms (primarily shooting pain, paresthesia’s and numbness).
Conclusions: With complex, multi-level injuries and complaints, it is imperative that a thorough
evaluation of all affected and related structures be performed by the attending clinician in order to
identify best practice and facilitate optimal functional outcomes. In this case, an interdisciplinary
approach between the surgeon and hand therapist that included the isolation of problematic structures
was a key component of identifying and resolving obstacles to the patient’s optimal function. The
patient reported increased general functional ability, reduced reliance on pain medication and
improved social participation. With complex, multi-level injuries and complaints, it is imperative that
a thorough evaluation of all affected and related structures be performed by the attending clinician in
order to identify best practice and facilitate optimal functional outcomes.
Keywords: Brachial Plexus, Adhesive Capsulitis, Compression, Myofascial Trigger Point,
Neurological, Musculoskeletal, Thoracic Outlet Syndrome, Incision, Scar Management
Brachial Plexus Injuries (BPIs) represent a significant source of disability, with impacts
ranging from motor weakness to debilitating pain, sensory deficits, and muscle atrophy. The
brachial plexus, formed by the cervical nerve roots C5 through T1, is highly susceptible to trauma,
with common etiologies including motor vehicle accidents, penetrating injuries, and falls [14,15].
Although spontaneous recovery is observed in many cases, a substantial proportion requires surgical
intervention, particularly in low-energy injuries where neurological complications are more frequent
[15]. Complicating the rehabilitation process, Thoracic Outlet Syndrome (TOS) often overlaps
with BPIs. This multifactorial condition, first described by Peet in 1956, involves compression of
neurovascular structures within the interscalene triangle and manifests through a constellation of
symptoms, including neck pain, paresthesia, and vascular disturbances [15]. While its incidence is
relatively low—3 to 8 per 1,000 individuals—diagnostic challenges persist due to the absence of a
definitive test, necessitating a nuanced clinical approach [6]. Further compounding these diagnoses,
adhesive capsulitis, or “frozen shoulder,” is frequently observed in patients recovering from upper
extremity injuries or surgeries, particularly in women and individuals over 50 years old [18,20].
Characterized by progressive loss of glenohumeral joint motion, this condition significantly impedes
rehabilitation efforts and requires targeted therapeutic interventions. This case study explores the
rehabilitation of a 57-year-old female patient with a complex diagnosis of brachial plexopathy, TOS,
and adhesive capsulitis following rotator cuff repair. Through a multidisciplinary approach combining
surgical and therapeutic interventions, the study highlights key strategies for addressing overlapping
musculoskeletal and neurological pathologies to optimize patient outcomes. By addressing critical
gaps in the treatment of multi-level injuries, this work aims to contribute to a growing body of
literature emphasizing individualized, interdisciplinary care models.
A 57-year-old right hand dominant female sustained a rotator cuff injury while shoveling snow in February
2021. In March of that year, she underwent a Rotator Cuff Repair (operative details not available). Postoperatively
she was immobilized in a brace. Within a week of surgery, she began to experience what she describes as
“scapular pain” specifically along the medial border. Upon consulting with the surgeon, the brace was adjusted
and she was informed by her medical team to expect no further complications. Physical Therapy (PT) began 4
weeks postoperatively and brace was discontinued. A few weeks after starting PT the therapist noted significant
lymphedema coupled with diffuse Right Upper Extremity (RUE) numbness and was referred to a lymphatic
massage specialist. The patient was unable to continue PT after July 2021 due to pain localized to the shoulder
and diffuse paresthesia’s throughout the right upper extremity. The patient did not recall any additional traumatic
injury preceding the exacerbation of symptoms. The patient stated that the distal RUE was never addressed in past
PT at a different facility despite a progression of symptoms including cyanosis, edema, paresthesia’s, numbness
and weakness while she was under their care. No specialized care or adjustment to th e therapy program occurred
despite the symptoms. Eight months after initial surgical intervention, she sought further evaluation from spine,
shoulder and hand specialists. Occupational limitations included difficulty with bathing, dressing, grooming,
driving, typing, meal preparation and sleep (see Table 1 for International Classification of Functioning, Disability
and Health codes). A course of Gabapentin had reduced the severity of some symptoms such as tremors and
paresthesia’s, but the pain, edema, stiffness and weakness persisted. The patient was understandably frustrated
with her functional deficits and inability to work.
According to her medical chart, the patient demonstrated no clavicular or atypical first rib anatomy.
Radiographic imaging of the patient’s cervical spine in September 2021 showed lower cervical degenerative disc
space narrowing and spondylosis with some mild right Acromioclavicular Joint (AC) degeneration. Magnetic
Resonance Imaging (MRI) in October 2021 revealed bilateral Plexi with symmetrical appearance, no abnormalities
in non-contrast multiplanar imaging, and no sign of root impingement at the cervical spine that would explain
distal symptoms of the extremity. There was minimal foraminal stenosis in spine levels C5-C7. Based on MRI
findings, epidural injection to the cervical spine was ruled out as a possible treatment. Muscle reflexes were normal
with no upper motor neuron signs. Hoffman sign was positive bilaterally, with Spurling sign positive only on the
right side with pain radiating to the posterior right scapula.
At initial hand therapy evaluation in November 2021, she presented with a constant pain level of 7/10 on the
Visual Analog Scale (VAS). Additionally proximal and distal neurological and motor symptoms were present
including a burning sensation at the medial border of the scapula and significant weakness when making a full fist
or grasping task tools during ADLS and IADLS. All active wrist and forearm motion in the right upper extremity
elicited tremors in the digits as well as and a burning sensation that radiated down the lateral side of the arm. The
patient also complained of periodic headaches that traveled from her shoulder up to the right side of her head. Upon
palpation, her right scalene and upper trapezius muscles were very Tight and Tender to Palpation (TTP). Objective
shoulder measures included active motion deficits of external/internal rotation, forward flexion (with a hard end
feel), extension and abduction compared to the contralateral side (see Table 2 for range of motion and strength
measures). The patient was also unable to perform pronation/supination, or wrist motion in all planes without
increased pain at the medial scapular border and tremors in the forearm and hand. Passive motion was not assessed
at her initial visit since it caused pain levels to rise to 10/10 on the VAS. Manual muscle testing showed weakness
with finger and elbow flexion, shoulder abduction as well as elbow and wrist extension with poor intrinsic hand
strength. Edema was evident at the right clavicular region and the patient’s entire extremity appeared swollen
and stiff. She was unable to work due to the severity of symptoms including constant pain, stiffness and tremors
throughout the extremity. Dermatome testing showed abnormal sensitivity with light touch and pinprick on the
lateral aspect of the RUE for C4, C5, C6, C8, T1 and T2 (Figure 2). Brachial plexus compression sites identified
during clinical examination included between anterior and middle scalene, palpation of these sites produced
vascular presentation observed with color and temperature changes in the extremity. Similar clinical findings
Occurred at end range external rotation of the shoulder capsule. Significant tenderness to palpation at the distal
end of sternum led to an investigation of the phrenic nerve (C3-C5) distribution since its path includes the anterior
surface of the anterior scalene muscle with proximity to the subclavian vein; this is particularly of note given
intermittent edema and skin changes that the patient was experiencing at the right clavicular region. End range
shoulder extension sometimes elicited pain at the right acromioclavicular joint which was tender with palpation.
The patient complained of increased pain and demonstrated tremors throughout the RUE with a persistently
poor ability to tolerate most treatment tasks that involved active wrist flexion and extension, forearm rotation,
elbow flexion to end range, glenohumeral joint external rotation, flexion and abduction. A comprehensive Home
Exercise Program (HEP) was provided that included modified ulnar, radial and median nerve glides and AROM
to address peripheral nerve irritation and joint stiffness. A trial of brachial plexus glides was deemed too painful
to add to HEP despite alterations to reduce the intensity of symptoms. Many of the wrist, forearm and shoulder
motion exercises were adapted for performance in the gravity-eliminated plane since that positioning elicited
the least amount of pain and minimal tremors. During the first 2 months of treatment, she had persistent pain
of 7/10 on the VAS localized to the medial border of the right scapula at baseline that was exacerbated by the
aforementioned movements. The hand therapist noticed that the application of a distal-to-proximal pull on the
skin at the extensor wad of the forearm reduced the severity of tremors and pain during active and passive motion,
perhaps due to addressing a deficient nerve/length tension relationship. Through palpation, joint mobilization as
well as trial and error it was noted that the application of compression in the form of Tubi grip size E just distal
to the radial head and at the spiral groove enabled the patient to perform up to 40 minutes of a therapy session
with reduced pain and tremors. Her pain responded most positively to alleviation of the downward pull of the
extremity with a brachial plexus sling (see Figure 3 & 4). These findings were relayed to the patient’s surgeon.
Who performed additional provocative testing and determined that a radial tunnel release procedure would be the
best strategy for addressing pain and weakness both distally and proximally. Prior to radial tunnel release surgery,
the patient had persistent pain throughout RUE from the medial border of the scapula radiating distally, periodic
paresthesia’s, intermittent edema and very limited functional use of the RUE unless the course of the radial
nerve was stabilized with compression and the application of distal-to-proximal traction. After the procedure,
she reported reduced pain, improved sleep quality and overall reduced symptoms despite weakness, stiffness
and limited use of RUE. An additional benefit to the radial tunnel release was that myofascial trigger points at
the shoulder and trunk formerly masked by high pain levels were more identifiable and resolvable using manual
therapy. Over the course of six weeks, the patient showed improvements in ROM throughout the extremity,
reduced pain and negligible tremors with end range motion of the shoulder. The most efficacious intervention was
the use of myofascial trigger point release at the anterior and middle scalene, as well as pectorals with an emphasis
In early April, two months after radial tunnel intervention, an increase in tremors in digits III, IV and V was
observed along with increased pain at the anterior shoulder along with a hard end feel for all external rotation
and abduction. This end feel was not presumed to be capsular in nature since muscle guarding of sufficient
intensity could mimic a similar effect. Subsequent to an examination by the shoulder specialist on the patient’s
care team, an arthroscopic capsular release was identified as the next course of action given her specific history
and a diagnosis of adhesive capsulitis due to postoperative contracture. A right glenohumeral capsular release
was performed in May 2022. During the procedure the rotator cuff repair was found to be intact with no biceps or
subscapularis pathology while arthroscopic lysis and debridement of identified lesions were performed under
general anesthesia. Status post-surgery motion was assessed to be: external rotation 45 degrees, internal rotation
30 degrees, forward flexion 110 degrees with a hard end feel and abduction 80 degrees. On the contralateral
side measures were 75, 65, 160 and 90 respectively. Hand therapy was resumed two days after the capsular release
due to surgeon concerns about regaining range of motion after 12 months of suboptimal movement.
At the 2-week post-operative follow up with the shoulder surgeon requested no ER stretch due to plexus symptomatology
that presented as tremors/paresthesia’s along the median and ulnar nerve distributions of extremity. Therapy focus
was then continued performance of fascia-release along the length of sternum with an emphasis on medial-to-lateral
traction on pectoral tissue. Although symptomatology and functional status improved, the patient continued to complain
of intermittent spasms, paresthesia’s and pain distal to the glenohumeral joint. In July of 2022, the patient underwent
a rib-sparing scalenectomy with pectoralis minor release with a supraclavicular approach with neurolysis of C4. The main
focus after this final surgical intervention was the management of scar tissue and preserving range of motion in an
extremity already prone to stiffness with scar from past surgeries present.
The patient was observed to demonstrate improved GHJ abduction and elevation post-trigger release and soft tissue mobilization,
especially when emphasis was placed on the serratus anterior, pectoral and axillary regions of the right rib cage. There was a dramatic
reduction in visible tremors of the RUE noted at end range GHJ abduction especially after focused serratus anterior trigger release.
Despite a thrice-weekly treatment schedule, the patient was unable to maintain therapeutic gains between sessions. Hence upon further
palpation of the entire trunk, additional trigger points were discovered on the contralateral side. These points responded positively to
a lateral-to-medial traction of the skin and underlying fascia, with the patient reporting a reduction of 2-3 points on the VAS when
ER and abduction were performed post-STM.
In order to lengthen the patient’s pain-free periods, she was educated to perform pectoral stretches on the contralateral side due to
noted tightness that limited all end range R GHJ motion away from midline. As her ability to lift the extremity away from midline improved,
additional trigger points were noted under R breast tissue that traveled from the diaphragm/bottom of sternum to the coracobrachialis region.
Additional trigger points were noted at the contralateral supraspinatus and infraspinatus that elicited tremors in right small and ring fingers
until released. The emphasis of this patient’s plan of care was to achieve tremor- and pain-free movement of the right upper extremity in
all planes to end-ranges. At the time of discharge, the patient reported improved sleep quality, increased ability to perform leisure tasks
that place upper extremities at the side of the body such as long walks, and reduced need for compensatory strategies when lifting and
carrying task objects. Paresthesia’s had reduced in intensity, albeit not eliminated completely and tremors were negligible when a manual
therapy macro-lens that included the contralateral chest wall enabled the patient to maintain ROM gains in the right GHJ without a return
of pain and tremors.
A mapping of the patient’s symptoms shows irritation of the medial cord of the brachial plexus, particularly the medial pectoral nerve,
ulnar nerve, as well as the posterior cord at the axillary and radial nerve. The manual muscle testing findings upon initial evaluation
indicate neurologic deficit at the lateral, medial, and posterior cords of the brachial plexus [12]. Trigger points at the axilla, scapula,
upper and middle trapezius, serratus anterior, rhomboids,
Pectorals, and latissimus dorsi compounded the patient’s pain and experienced neurological deficits. When active
myofascial trigger points and glenohumeral pathologies present in tandem, they pose significant challenges for
therapists treating Thoracic Outlet Syndrome (TOS) [23]. Effective treatment approaches for brachial plexopathy
and TOS often require a multidisciplinary strategy incorporating surgical and non-surgical interventions. Ribsparing
scalenectomy, as demonstrated by Johansen (2021), achieved significant symptom relief, with 90.9% of patients
experiencing more than a 50% improvement in functionality and a reduction in Quick DASH scores from 62.6 to 25.2
postoperatively. This approach effectively addressed fibrotic and contracted scalene muscles without the need for
first rib resection, highlighting the potential of focused soft tissue decompression to alleviate neurogenic symptoms.
Similarly, the trans axillary incision approach, while less invasive and preserving cosmetic outcomes, has shown
variable results depending on the depth of neurovascular decompression and its ability to minimize postoperative
complications [21]. In this case, the suspected Diagnosis of Disputed Neurogenic Thoracic Outlet Syndrome
(Danto’s), as indicated by negative EMG findings despite clear neurological symptoms (Stewman, 2014), underscores
the complexity of accurately diagnosing and managing overlapping neurovascular compressions. This classification
allowed a more targeted treatment approach, including the application of customized braces to reduce strain and
promote stability. Notably, a single therapy visit involving customized bracing resulted in a 50% reduction in pain
by stabilizing the Arcade of Frohs and spiral groove of the humerus, which aligns with the therapeutic principles
of optimizing the length-tension relationship of nerve structures [15,13]. For more localized compressions, such as
pectoralis minor syndrome, [5] demonstrated the efficacy of arthroscopic pectoralis minor tendon release, which
improved pain scores (VAS reduction from 8.5 to 1.0) and functional outcomes such as Quick DASH scores decreasing
from 83.1 to 19.3. This aligns with the patient’s improved outcomes following targeted manual therapy and myofascial
release focused on pectoral structures.
Diagnostic imaging revealed no structural abnormalities of the brachial plexus, emphasizing the importance of
functional and symptom-based assessments. Utilizing the Gate theory of pain modulation, the therapeutic priority
was lowering pain levels (VAS ≥7/10 for six months) to reduce sympathetic nervous system activation, thereby
improving patient receptivity and functional outcomes. Sympathetically maintained pain, driven by heightened
norepinephrine release, further validated the need for interventions targeting both physical and neural mechanisms
[19]. Scar management also played a critical role in optimizing outcomes, as highlighted by [22]. Effective scar
management not only improves cosmetic appearance but also mitigates functional impairments caused by adhesions and
restricted tissue mobility. Techniques such as manual scar mobilization and compression therapy can reduce the risk
of tethering, which is especially relevant for patients undergoing surgeries like rib-sparing scalenectomy and
arthroscopic tendon release. This approach ensures that the soft tissue structures surrounding the brachial plexus
and thoracic outlet remain pliable, reducing the likelihood of re-injury or functional limitations.
At discharge, a collaborative effort between therapist and patient led to the creation of a minimalist neural
structure support, effectively managing tremors and scapular pain. The integration of surgical, therapeutic, and
adaptive strategies facilitated this patient’s progress. Empowering the patient as an active participant in their
recovery was critical, mitigating frustration and fostering resilience in the face of prolonged symptoms. This case
underscores the imperative for a responsive, interdisciplinary care team to address the multifaceted nature of TOS
and brachial plexopathy, ensuring timely and comprehensive interventions. By maintaining clear communication between
the patient and surgical teams, the hand therapist was able to optimize outcomes and pave the way for further functional recovery.
Thank you to the following for generous contributions of their time, support and feedback in the development of
this case report: Michael Rivlin MD and Michael Mueller OT, CHT of the Rothman Orthopedics Institute Philadelphia, PA U.S.A,
Rodney French MD, MEd, FRCSC, Dip Sports Med of the Specialist Referral Clinic, Vancouver B.C Canada.
An Interdisciplinary Approach in the Rehabilitation of a Triple Diagnosis of Brachial Plexopathy, Thoracic Outlet Syndrome and Adhesive Capsulitis
Certified Hand Therapist Rothman Orthopedic Institute Philadelphia, PA.

Abstract
Introduction
Patient Information
Diagnostic Assessment
Clinical Findings
Therapeutic Intervention
Outcomes
Discussion
Diagnostic Findings
Collaborative Effort
Acknowledgements
References



