Abstract
Background: Pediatric Emergence
Delirium (PED) is common after General Anesthesia
(GA) in children, characterized by agitation and
confusion. Though brief, it can cause injury,
distress, and prolonged hospital stays. This study
aimed to assess the incidence and associated factors
of PED in children undergoing ENT surgery at Tikur
Anbessa Specialized Hospital (TASH), Addis Ababa,
Ethiopia.
Objectives: To determine the
incidence of PED and identify associated risk
factors in pediatric patients undergoing ENT
surgeries under GA.
Method: A prospective
cross-sectional study was conducted from September
2023 to April 2024. A total of 88 children aged 2–12
years undergoing elective ENT surgeries were
included. Data were collected using a structured
questionnaire. The Pediatric Anesthesia Emergence
Delirium (PAED) scale was used to assess PED, with a
score ≥12 indicating PED. Binary logistic regression
identified predictors of PED.
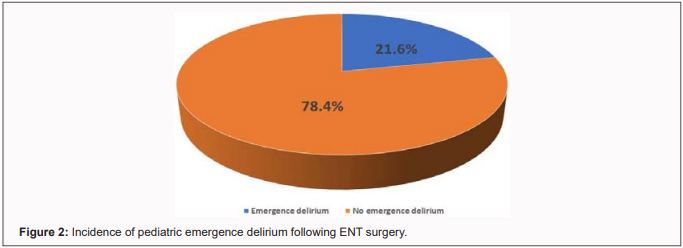
Results: The incidence of PED was
21.6%. Significant risk factors included toddler and
preschooler age (AOR=4.83, p=0.039), preoperative
maladaptive behavior (AOR=12.16, p=0.003), lack of
premedication (AOR=0.11, p=0.043), and moderate to
severe postoperative pain (AOR=11.05, p=0.005).
Recommendations: Premedication
should be routinely administered to reduce PED risk.
Preoperative maladaptive behaviors need to be
addressed, and effective pain management strategies
should be implemented. Additionally, caregivers
should be educated about PED to enhance their
understanding and support during the recovery
process.
Keywords
Emergence Delirium, Pediatric Anesthesia, ENT
Surgery, Risk Factors, Postoperative Pain
Introduction
Emergence Delirium (ED)
is a brief period of agitation commonly observed
in children during emergence from General
Anesthesia (GA). This can manifest as
disinhibition, restlessness, crying, and
confusion, often resolving shortly after removal
of noxious stimuli like the endotracheal tube.
However, some children may experience
postoperative delirium that persists or recurs
after initial emergence from anesthesia, or may
only become evident in the Post-Anesthesia Care
Unit (PACU).
Postoperative delirium can be categorized into
two subtypes: hyperactive, characterized by
agitation, and hypoactive, where the child is
somnolent and mentally altered. In pediatric
patients, ED is more prevalent compared to
adults. It is defined as a dissociative state of
consciousness where the child may be irritable,
uncooperative, incoherent, and inconsolably
crying, moaning, or thrashing.
While “emergence agitation” and “emergence
delirium” are often used interchangeably,
agitation typically refers to mild-to-moderate
distress without significant cognitive changes,
whereas delirium involves confusion and
disorientation. Delirium can also occur without
agitation, in a hypoactive form, where the child
may appear quiet, withdrawn, and unaware of
their surroundings.
ED in children is particularly common in the
PACU, where affected children may move
aimlessly, avoid eye contact, or behave
abnormally. They may also pull at IV lines,
monitors, and dressings. Although clinical
observation remains central to diagnosis,
several scales, including the Watcha, Cravero,
and Pediatric Anesthesia Emergence Delirium
(PAED) scales, have been developed.
The PAED scale, introduced in 2004, is the most
widely used tool for diagnosing ED, with a score
of 12 or above offering the highest diagnostic
sensitivity and specificity. Children with ED
are at increased risk of disrupting surgical
repairs and dislodging tubes or catheters,
presenting safety concerns both for themselves
and PACU staff. Additionally, ED often leads to
the need for increased staffing, which may
strain PACU resources.
Parental concern is heightened, as children with
ED are 1.4 times more likely to experience
maladaptive behavioral changes, such as
separation anxiety and sleep disturbances,
lasting up to two weeks postsurgery. While ED is
recognized globally, there is a significant gap
in research regarding its incidence in children
undergoing ENT surgeries, particularly in
African countries like Ethiopia.
This study aims to address this gap by assessing
the incidence of PED in children undergoing ENT
surgeries at Tikur Anbessa Specialized Hospital
(TASH), Addis Ababa. The findings will help
identify risk factors and guide early
interventions, improving perioperative care and
providing data for further research in pediatric
anesthesia management.
Objectives
To assess the incidence
and associated factors of emergence delirium in
pediatric patients undergoing ENT surgery under
general anesthesia in TASH.
Study Area and Period
The study was conducted
at Tikur Anbessa Specialized Hospital, Addis
Ababa University, College of Health Sciences.
TASH is the largest referral hospital in
Ethiopia, offering specialized clinical services
not available in other public or private
institutions in the country. The study period
spanned from September 1, 2023, to April 30,
2024.
Study Design
This was an
institutional-based Prospective Cross-Sectional
Study aimed at assessing the incidence of
Emergence Delirium (ED) and identifying
associated risk factors in pediatric patients
undergoing ENT surgeries under General
Anesthesia (GA). The study observed patients in
the postoperative period, with data collected
during their stay in the PACU and through
follow-up assessments.
Population
Source population: All pediatric
patients who underwent surgery under general
anesthesia in Tikur Anbessa Specialized
Hospital.
Study population: All pediatric
patients 2–12 years of age who underwent ENT
surgery under GA in TASH during the study period
that met the inclusion criteria.
Eligibility Criteria
Inclusion Criteria
Pediatric patients aged 2–12 years, classified as ASA
I, II, or III who underwent elective ENT surgery
under General Anesthesia (GA) during the study
period.
Exclusion Criteria:
- Patients who are mechanically ventilated for a prolonged period following surgery.
- Patients transferred to the Intensive Care Unit (ICU) after surgery.
- Patients diagnosed with cognitive developmental delay.
Sampling
Sample size and Sampling techniques:
A total of 88 pediatric patients who have undergone
elective ENT surgery between the period of September
2023 and April 2024 in TASH were included in the
study using the Consecutive sampling technique.
Variables
Independent: Age, Sex, ASA class,
Comorbidity/Coexisting disease, Preoperative
behavior, Premedication, Type of anesthesia,
Anesthesia duration, and Postoperative pain
Dependent: Emergence delirium
Data Collection
After receiving informed oral consent, the data was
collected using a standardized questionnaire. The
data was gathered starting from the immediate
post-extubating period in the OR and then in the
PACU by the principal investigator, anesthesiology
residents, and anesthetists assigned to the ENT OR
table. PAED scale was used to assess for ED and a
PAED scale of 12 or more was taken as PED.
Operational definition
- Maladaptive behaviors – behavior that prevents an individual from adjusting well to certain situations. This behavior includes anxiety, withdrawal, agitation, uncooperative behavior, temper tantrums, or aggressions.
- Premedication – administration of medications to patients before induction of general anesthesia for a surgical procedure to reduce their anxiety, induce sedation, or prevent pain.
- Cognitive developmental delay – condition in which children lag in intellectual functioning and whose behavior and communication are significantly below expectations.
- Pediatric emergence delirium – patients with a PAED score of 12 or more were taken as having emergence delirium.
- FLACC pain scale – is a behavioral pain assessment scale scored 0-10 where 0 = relaxed and comfortable, 1-3 = mild discomfort, 4-6 = moderate pain, 7-10 = severe pain or discomfort.
Data Analysis and Procedures
The data collected was reviewed by the main investigator and checked for quality and any missing documents before data input and analyzed manually using SPSS version 26 software. Bivariate logistic regression analysis was carried out to examine the predictors of the outcome variable. Variables with a p-value of < 0.25 on bivariant logistic analysis were taken to multivariable logistic regression analysis and a p-value of less than 0.05 was taken as a statistically significant predictor of postoperative delirium. The Hosmer-Lemeshow goodness of fit test was used to evaluate the appropriateness of the logistic regression model, with p > 0.05. Descriptive statistics was done for all variables and the results are presented in tables, graphs, and pie charts.
Data Quality Assurance
The data collectors were briefly trained before data collection on pediatric emergence delirium and there was a daily meeting during the data collection to clear up any ambiguity. The data collected from the questionnaire was reviewed by the main investigator and checked for completeness every day.
Ethical Considerations
The study participants and their attendants were informed about the aim of the study before the data collection began and that they were able to withdraw from the study at any point during the research, then oral consent was obtained from each patient’s parents or legal guardians. To ensure confidentiality, no patient identifiers were used in the data collection process. Instead, each participant was assigned a unique code number to maintain anonymity. Ethical clearance and support letter were obtained from Addis Ababa University College of Health Science Department of Anesthesiology, Critical Care and Pain Medicine and submitted to Tikur Anbessa Comprehensive Specialized Hospital Chief Clinical and Academic Director Offices.
Dissemination
Results to be shared with academic institutions, hospitals, and health bureaus, published in journals, and presented at workshops.
Results
Sociodemographic and
Preoperative Data
A total of 88 pediatric
patients who underwent elective ENT surgery between
September 2023 and April 2024 at Tikur Anbessa
Specialized Hospital (TASH) were included in the
study. Of these, 31 (35.2%) were toddlers and
preschoolers, while 57 (64.8%) were school-aged
children. The sample included 42 (47.7%) females and
46 (52.3%) males.
Regarding coexisting conditions, 59 (67%) had no
coexisting diseases, while 29 (33%) had other
coexisting medical conditions. In terms of
preoperative management, 19 (21.6%) were
premedicated with ketamine. Behaviorally, 51 (58%)
of the children were calm, while 37 (42%) displayed
maladaptive behavior during separation from their
parents in the waiting room (Table 1).
Intraoperative Data
During induction in the OR,
29 (33%) were calm, 44 (50%) had maladaptive
behavior, and 15 (17%) were previously sedated in
the waiting room area. All 88 patients were given
inhalational anesthesia as maintenance of
anesthesia.
69 (78.4%) of the patients had surgery duration of
less than 45 minutes and anesthesia duration of less
than 1 hour, compared to 19 (21.6%) patients whose
surgery and anesthesia duration was greater than 45
minutes and 1 hour respectively (Table 2).
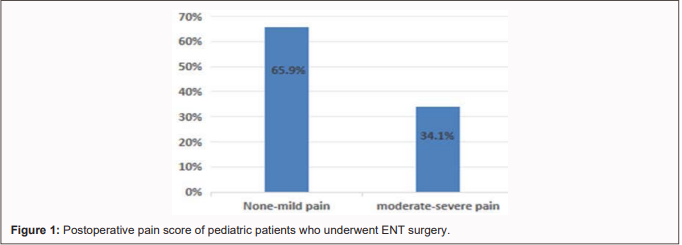
Postoperative Data
None of the 88 patients who
underwent surgery had vital sign derangement in the
PACU. 58 (65.9%) had mild or no pain in contrast to
the 30 (34.1%) who experienced moderate to severe
pain. Out of the 88 patients, 19 (21.6%) had ED
(Table 3).
Factors Associated with
Pediatric Emergence Delirium Following ENT Surgery
To test the relationship between pediatric emergence
delirium and the independent variables, bivariate
binary logistic regression analysis was performed on
selected independent variables with the dependent
variable. Variables having a p-value of < 0.25
were selected and then included in the multivariable
logistic regression analysis. These variables were
age, sex, the behavior of the patient during
parental separation, premedication, anesthesia
duration, and post-operative pain scale in the PACU.
The odds of developing emergence delirium were 4.8
times higher in toddlers and preschoolers [AOR=4.831
(95% CI: 1.08–21.62)] compared to school-age
children. Patients with maladaptive behavior like
anxiety, agitation, and restlessness were found to
be 12 times more at risk of pediatric emergence
delirium [AOR=12.16 (95% CI: 2.278–64.91)] compared
to those who were calm during their separation from
parents in the waiting room area.
Those patients who were premedicated before
induction of anesthesia were 89% less likely to
develop emergence delirium [AOR=0.11 (95% CI:
0.013–0.928)] than those who did not receive
premedication. Patients with moderate to severe pain
postoperatively were 11 times more likely to have
emergence delirium [AOR=11.05 (95% CI: 2.058–59.34)]
compared to those with mild or no pain in the PACU.
(Table 4)
Discussion
Emergence Delirium (ED) is a
common occurrence in pediatric patients in the
post-anesthesia care unit (PACU), with an overall
incidence ranging between 10% and 80% across various
procedures. In this study, the prevalence of ED was
21.6%, aligning closely with previous findings from
Michigan, USA (18%), Iran (17.9%), Germany (23%),
and South Asia (22.4%). However, studies focusing on
pediatric patients undergoing ENT surgeries have
reported a broader range of incidences, from as low
as 1.3% at the University of Texas to as high as 56%
in Turkey. These variations may be attributed to
differences in patient demographics, preoperative
anxiety levels, anesthetic management, and study
methodologies. Age emerged as a significant risk
factor for ED in this study, with toddlers and
preschool-aged children displaying a higher
likelihood of experiencing delirium upon emergence
from anesthesia (p=0.039). This finding aligns with
a retrospective study from the University of Texas
Southwestern Medical Center, which reported that
toddlers had a higher prevalence of ED than
preschoolers (p=0.04), middle-aged children
(p<0.001), and teenagers (p=0.01). Similarly, a
prospective observational study in Addis Ababa found
that children aged 2–6 years were twice as likely to
develop ED compared to those aged 7–12 years
(p=0.042). The increased susceptibility in younger
children may be due to their limited ability to
comprehend and communicate their emotions,
heightened separation anxiety, and immature
cognitive development, all of which contribute to
elevated stress levels.
Contrary to a retrospective study from the
University of Texas Southwestern Medical Center and
a prospective observational study in India, both of
which reported a higher prevalence of ED in boys
(p=0.03 and p=0.04, respectively), our study found
no significant association between male gender and
ED (p=0.071). This discrepancy may be due to
differences in anesthesia duration between genders
in previous studies, whereas in our study, both
sexes had comparable anesthesia times. Additionally,
the Indian study had a male-dominated sample (82.4%
boys vs. 17.6% girls), whereas our study had a more
balanced gender distribution (52.3% boys vs. 47.7%
girls). Supporting our findings, an observational
study conducted in South Asia also did not establish
a significant correlation between gender and ED.
Preoperative anxiety and maladaptive behaviors
during parental separation in the waiting area
significantly influenced the incidence of ED
(p=0.003). Children exhibiting agitation, anxiety,
restlessness, uncooperativeness, and exaggerated
displays of anger were more likely to develop ED.
Similar findings were reported in studies conducted
in South Asia (p=0.0005), Iran (p<0.005), Amhara
(p=0.02), and India (p=0.01). The underlying
mechanism may be related to the increased stress
levels and emotional dysregulation in children with
maladaptive behaviors, which could heighten their
susceptibility to delirium during the recovery
phase.
The use of premedication significantly reduced the
likelihood of ED in our study (p=0.043). Similar
results were reported in a study from Turkey, where
children who received oral ketamine premedication
had an 18% incidence of ED compared to 56% in those
who did not receive premedication (p=0.001). A study
in the Amhara region also found that sedative
premedication reduced the risk of ED by 58%
(p=0.007). The anxiolytic and sedative effects of
premedication may help stabilize the emotional state
of pediatric patients before surgery, thereby
reducing stress and the subsequent risk of delirium.
Postoperative pain was strongly associated with the
occurrence of ED in our study (p=0.005). Patients
experiencing moderate to severe pain in the PACU
were 11 times more likely to develop ED. These
findings are consistent with studies conducted in
Iran (p<0.0005), Amhara (p<0.001), and India
(p=0.002), all of which identified pain as a
significant risk factor for ED. One possible
explanation is that pain disrupts normal brain
function, increasing susceptibility to
neurocognitive disturbances such as delirium.
Some studies have reported a correlation between
shorter anesthesia durations and increased ED
incidence. However, our study did not find a
significant association (p=0.943). Differences in
anesthetic agents and techniques may account for
these discrepancies. While some studies suggest that
rapid emergence from anesthesia predisposes patients
to delirium, variations in study methodologies and
anesthetic protocols may explain the conflicting
findings.
Strength of the Study
The study design was a prospective study which
increases the ability of this research to
establish stronger evidence of causality between
factors and the emergence of delirium. Even
though there are several rating scales for the
assessment of PED, this study used the PAED
scale, which is the accepted standard for the
diagnosis of emergence delirium in children. The
study tried to identify pediatric patients at
risk of developing ED, which can help anesthesia
providers to work on its prevention.
Limitations of the Study
Even though a valid and reliable tool was used to
diagnose emergence delirium in pediatrics, the
PAED scale, due to its subjective nature may
cause or introduce inter-rater variability due
to differences in interpretation among different
observers. Due to the poor standard of the PACU
and scarcity of resources, confounding factors
of ED like hypoglycemia and hypotension could
not be ruled out in patients using objective
blood glucose and blood pressure measurements.
Instead, pulse rate and capillary refill were
used to identify hypotension, and other signs
and symptoms of hypoglycemia were looked for to
rule out hypoglycemia. The study was conducted
in a single center with a small sample size, so
the generalizability of the findings to broader
pediatric populations may be limited.
Conclusion and
Recommendation
Conclusion
The incidence of ED in pediatric patients
undergoing ENT surgery in TASH was found to be
21.6%. This study also highlights several
factors emerging as significant predictors of ED
in the toddler and preschooler age group, with
preoperative maladaptive behaviors, lack of
premedication, and postoperative pain being
highly associated with developing postoperative
PED.
Recommendation
Conducting thorough preoperative evaluations to
identify patients at increased risk of ED,
providing psychosocial support to patients
throughout the perioperative period,
administering premedication to patients with
high levels of anxiety in the preoperative
period, giving multimodal analgesia to minimize
perioperative discomfort or pain, and developing
hospital protocols to promptly identify and
manage ED in the PACU are recommended based on
this study.
Further multicenter studies should be done in
the pediatric population to work towards
reducing the incidence of ED, identifying any
additional risk factors for ED, enhancing pre-
and postoperative anesthetic management, and
improving the overall perioperative experience
for pediatric patients.
References
-
1.
Lerman J,
Davidson A, Crowley M. Emergence
Delirium and agitation in children.
UpToDate. 2018;1–21.
-
2.
Reduque LL,
Verghese ST. Paediatric emergence
delirium. Continuing Education in
Anaesthesia, Critical Care and Pain.
2013;13(2):39–41.
-
3.
Paediatric
emergence delirium - ResearchGate.
-
4.
CA L.
Paediatric Emergence Delirium: An
Approach to Diagnosis and Management in
the Postanaesthesia Care Unit. Journal
of Perioperative & Critical Intensive
Care Nursing. 2018;04(01):2–4.
-
5.
Lee
C. Paediatric Emergence Delirium: An
Approach to Diagnosis and Management in
the Postanaesthesia Care Unit. J
Perioper Crit Intensiv Care Nurs.
2017;04(01).
-
6.
Yu H,
Sun X, Li P, Deng X. Prevalence and risk
factors of emergence agitation among
pediatric patients undergoing ophthalmic
and ENT Surgery: a cross-sectional
study. BMC Pediatr. 2023 Dec
1;23(1).
-
7.
Voepel-Lewis
T, Malviya S, Tait AR. A prospective
cohort study of emergence agitation in
the pediatric postanesthesia care unit.
Anesth Analg. 2003 Jun
1;96(6):1625–30.
-
8.
Postanesthetic
Emergence Agitation in Pediatric
Patients under General Anesthesia -
PubMed [Internet]. [cited 2025 Jan
30].
-
9.
Houben A,
Ghamari S, Fischer A, Neumann C, Baehner
T, Ellerkmann RK. Pediatric emergence
delirium is linked to increased early
postoperative negative behavior within
two weeks after adenoidectomy: an
observational study. Brazilian Journal
of Anesthesiology (English Edition).
2024 Sep 1;74(5).
-
10.
Ali
AB, Khan F. Emergence Delirium and Its
Association with Preoperative Anxiety in
Paediatric Patients Undergoing Infra
Umbilical Surgery Under Combined General
and Caudal Anaesthesia: An Observational
Study from a Tertiary Care Centre in a
South Asian Country. Turk J Anaesthesiol
Reanim [Internet]. 2022 Apr 1 [cited
2025 Jan 30];50(2):129–34.
-
11.
González-Cardenas
VH, Munar-González FD, Pinzón-Villazon
IL, Cabarique-Serrano SH,
Burbano-Paredes CC, Cháves-Rojas N, et
al. Study of paediatric postoperative
delirium and acute pain in low surgical
risk procedures. Colombian Journal of
Anesthesiology. 2018 Mar
1;46(2):126–33.
-
12.
Liu
K, Liu C, Ulualp SO. Prevalence of
Emergence Delirium in Children
Undergoing Tonsillectomy and
Adenoidectomy. Anesthesiol Res Pract
[Internet]. 2022 [cited 2025 Jan
30];2022.
-
13.
Kararmaz A,
Kaya S, Turhanoglu S, Ozyilmaz MA. Oral
ketamine premedication can prevent
emergence agitation in children after
desflurane anaesthesia. Paediatr Anaesth
[Internet]. 2004 [cited 2025 Jan
30];14(6):477–82.
-
14.
Teketel A.
The Incidence and Associated Risk
Factors of Emergence Agitation in
Pediatric Patients after General
Anesthesia at Addis Ababa Governmental
Hospitals from February-May 2021
(Prospective Observational Study)
[Internet]. 2021 [cited 2025 Jan
30].
-
15.
Devi
EA, Nagaprasad YVSR, Shiva P V.,
Nirmalan P. Incidence and risk factors
for emergence delirium in children
undergoing surgery under general
anaesthesia - A prospective,
observational study. Indian J Anaesth.
2023 Aug 1;67(8):725–9.
-
16.
Postanesthetic
Emergence Agitation in Pediatric
Patients under General Anesthesia -
PubMed [Internet]. [cited 2025 Jan
30].
-
17.
Ali
AB, Khan F. Emergence Delirium and Its
Association with Preoperative Anxiety in
Paediatric Patients Undergoing Infra
Umbilical Surgery Under Combined General
and Caudal Anaesthesia: An Observational
Study from a Tertiary Care Centre in a
South Asian Country. Turk J Anaesthesiol
Reanim [Internet]. 2022 Apr 1 [cited
2025 Jan 30];50(2):129–34.
-
18.
Yaregal
Melesse D, Teshale Tesema T, Ayinie
Mekonnen Z, Chekol WB, Admass BA, Mengie
Workie M. Predictors of postoperative
delirium in paediatric patients
undergoing surgery under general
anaesthesia at Amhara Regional State
Tertiary Hospitals: a multicenter
prospective study. Front Pediatr
[Internet]. 2024 Mar 8 [cited 2025 Jan
30];12.