Abstract
Background
Adhesive small bowel obstruction develops in 2.4% of all abdominal procedures due to intra-abdominal adhesions.
This is a common surgical emergency that results in severe morbidity and, in some cases, fatality.
Non-operative management of adhesive SBO has claimed success rates of 70–90%; surgical treatment is unavoidable
with unresolved obstruction under this management. The cut-off time to declare failed conservative management is
controversial. In our setup, we are using 72 hrs. as a cutoff point to declare failed conservative management,
and there is a lack of evidence on the management outcome and associated factors of such patients.
Objectives
The aim of this study was to evaluate the outcome of non-operative management of adhesive small bowel obstruction
and associated factors at Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, 2022.
Methods
A cross-sectional study was conducted on 183 patients treated for adhesive small bowel obstruction
from April 2016 to August 1, 2022. A retrospective review of the clinical records was performed
to collect data on sociodemographic, clinical, and management data using a data extraction form.
The collected data were then cleaned and entered into SPSS for analysis.
Mean and interquartile range were used for continuous variables, and frequency and percentage for categorical variables.
Adjusted Odds Ratio (AOR) with a 95% confidence interval and
p-value < 0.05 were used to declare statistically significant variables.
Result
Most of the patients were men (60.1%) and the median age of subjects was 45 years
(IQR-15–95 years). Hundred twenty-six (68.9%) of the patients were from the urban area while 57 (31.1%) came from rural areas. The mean duration of symptoms before admission was 32.64 hrs
(SD-26.4). Successful outcome obtained in 93 (50.8%) patients and the remaining patients had failure
of resolution after 72 hours or clinical deterioration resulting in operative management. The lengths of stay were found to be 4.71 days, 8.78 days and 13.48 days respectively for successful, failure to resolve at 72 hrs.
and clinical deterioration during conservative management respectively. On multivariate regression, the predictors of failed conservative management were having WBC > 11k at time of admission, having previous procedure of colorectal and gynecologic surgery, tenderness at presentation and signs of intra-abdominal collection at admission.
Conclusion
ADSBO is common and conservative management is first line of management.
Health care givers should take strict follow up during conservative management. In our study special attention should be given for patients who have
leukocytosis (WBC >11K), gynecologic and colorectal surgery, signs of collection and tenderness at presentation because they have a significant association with failed conservative management.
Keywords
Adhesive Small Bowel Obstruction (ADSBO), Non-operative management, Surgical treatment, Risk factors, Conservative management outcomes.
Acronyms and Abbreviations
ADSBO - Adhesive small bowel obstruction,
SPHMMC - Saint Paul’s Hospital Millennium Medical College,
PI - Principal investigator,
SPSS - Statistical package for social science,
MD - Medical doctor,
DC - Data collector,
OPD - Out patient department,
E.C - Ethiopian calendar,
NGT - Nasogastric tube,
NOM - Non operative management,
SBO - Small bowel obstruction,
Hrs - Hours,
DM - Diabetes mellitus,
HTN - Hypertension,
CLD - Chronic liver disease,
CKD - Chronic kidney disease,
RVI - Retroviral infection.
Introduction
Adhesive small bowel obstructions are obstructions due to intra-abdominal adhesions related
to prior abdominal surgery. Adhesive Small Bowel Obstruction (ADSBO) is a common surgical
emergency, causing high morbidity and at times mortality. Intra-peritoneal adhesions or bands, which
can begin forming within a few hours after an operation, causing such bowel obstructions are typically the footprints of previous abdominal surgical procedure, represent a life-long issue [1]. The incidence of Adhesive Small Bowel Obstruction (ADSBO) following all types of abdominal operations was 2.4% [2]. A significant amount of time and money has been invested into research on intra-abdominal adhesions, with a primary focus on the development of methods to prevent their formation. [3] Intra-abdominal adhesions related to prior abdominal surgery account for up to 75% of cases of small bowel obstruction. Over 300,000 patients are estimated to undergo surgery to treat adhesion-induced small bowel obstruction in the United States annually [4]. In Ethiopia, ADSBO is one of the raising causes of SBO and emergency admissions. According to a study done in Nekemte Hospital, ADSBO is the leading cause of SBO which attributes to 35% of SBO.
ADSBO is clinically diagnosed in a patient with intermittent colicky abdominal pain, distention, and nausea (with or without vomiting), with or without absence of stools. Other causes of SBO like hernia, intussusception, and tumor obstruction should be excluded. In patients with incomplete obstruction, watery diarrhea may be present. Stool may present in some patients with high obstruction; thus, good clinical assessment should be done to avoid misdiagnosis. History taking and physical examination have a low sensitivity for detecting bowel strangulation and ischemia, so close follow-up should be done with additional radiologic and laboratory parameters [1].
Current helical CT scans not only have good test characteristics for diagnosing small bowel obstruction but also have approximately 90% accuracy in predicting strangulation and the need for urgent surgery and also exclude other causes of SBO. Conservative management should always be tried in patients with adhesive small bowel obstruction, unless there are signs of peritonitis, strangulation, or bowel ischemia [7]. Conservative management is effective in approximately 70–90% of patients with ADSBO. Duration of the period in which conservative management can be tried is subject to debate, but most authors and the panel consider a 72-h period as safe and appropriate [1].
Conservative management might include any or all of the following: no oral intake; decompression by nasogastric intubation; intravenous fluids, with electrolytes as needed; and follow-up abdominal x-rays (usually daily) [5]. Close follow-up of abdominal conditions and vital signs, serial monitoring of input and output should be carried out. The use of Gastrografin® in patients with adhesive small bowel obstruction helps in earlier resolution of obstruction and reduces the length of hospital stay. It’s both diagnostic and therapeutic. Also, it predicts the likelihood of being successful in conservative management. If contrast reaches the colon after 24hrs of contrast ingestion, it shows the obstruction is highly likely to respond non-operatively.
Operative management/surgery is indicated in patients with clinical deterioration (signs of strangulation) or with radiological evidence of strangulation or failed conservative management. Operative management is found to slightly reduce the risk of future recurrence and is associated with an increased risk of morbidity and mortality [5]. Another option for operative management is the laparoscopic approach. Although patient selection is the strong key factor for having success in laparoscopic approach, it improves postoperative outcomes and functional recovery, and should be considered in patients in whom simple band adhesions are suspected. Conversion rate to open surgery was 38.5% [6]. Laparoscopic adhesiolysis should only be performed in high-volume centers with specific expertise in emergency laparoscopy, especially in tertiary referral centers with availability of operating room and laparoscopic equipment at all times, and with highly trained surgical and OR staff [7].
There is no guideline which recommends direct operative management unless the above indications appear.
Statement of The Problem
Intra-abdominal adhesions reduce quality of life and place an additional strain on health-care resources in low-income countries. Re-operations are made more difficult because there is a greater risk of iatrogenic bowel injury during surgery. Furthermore, repeated laparotomy and adhesiolysis results in the formation of even more adhesions. In Sweden, the annual health-care burden from adhesive disease is estimated to be $13 million [2]. The frequency of small intestinal obstruction following post-operative adhesions is increasing not only in developed countries but also in developing countries. ADSBO is a common cause of hospitalization in emergency departments, accounting for 4% of all admissions and 20% of emergency surgical procedures
[9]. ADSBO causes significant impact on health care, with an average stay in the hospital of 8 days and a 3% in-hospital mortality rate per episode [10]. Many studies recommend that conservative approach allows resolution of obstruction in most of the cases although recurrence is common. They also suggest that surgery is not curative and surgery cannot prevent recurrence also. Recommendations and success rate of non-operative management are quite variable across setups and countries. There are limited studies conducted on conservative management outcomes of ADSBO and associated factors in our setup despite the fact that it has been progressively increasing in prevalence. Hence, this study aims to assess the management outcomes of conservatively managed adhesive small bowel obstruction and associated factors in patients at the surgical department of SPHMMC.
Significance of the Study
Given that there is paucity of published studies on the conservative management outcome and associated factors of ADSBO, this study will provide local data about conservative management outcomes and associated factors of ADSBO for the scientific community. In SPHMMC, the outcome of non-operative management and associated factors is not studied. This study can also be a baseline for further study and can be an asset to develop management guideline.
Literature Review
The incidence of Adhesive Small Bowel Obstruction (ADSBO) following all types of abdominal operations was 2.4 percent in a comprehensive review and meta-analysis done to examine the burden of adhesion in abdominal and pelvic surgery. The evaluation included 87 papers with 110,076 participants. This rate varies depending on the patient’s age, location, and type of surgery. Pediatrics (4.2%) and lower gastrointestinal surgery (3.2%) had the highest rates, whereas abdominal wall surgeries (0.5%) and upper gastrointestinal surgeries had the lowest rates (1.2 percent). The rate of ADSBO after laparoscopic surgery was only 1.4 percent, which is quite low. Adhesions appeared to be the most common cause of postoperative small intestinal obstruction, accounting for 56 percent (49 percent to 64 percent; I2=96 percent) of cases in 42 investigations (including 5390 patients) [4]. Two district hospitals in the United Kingdom, Colchester General Hospital and Joyce Green Hospital, conducted a retrospective study to analyze ADSBO treatment patterns and associated costs in 110 hospital admissions. 41 (37%) of the 110 hospitalizations were surgically treated, whereas 69 (63%) were handled conservatively. The mean (SD) length of stay for surgical treatment was 16.3 days (11.0 days) and 7.0 days (4.6 days) for conservative treatment. The surgical group had a 9.8% in-patient mortality rate, while the conservative group had a 7.2 percent rate [8]. In another systematic review and meta-analysis done in UK, North Manchester general hospital comparing outcomes of operative vs non-operative management of ADSBO; operative management was associated with a lower risk of future recurrence but a higher risk of mortality and complications. There was comparable result in length of hospital stay and need for surgical re-intervention in both operative and non-operative [6]. In a 6-month prospective descriptive study conducted in Bangladesh in the Surgery Department of Rajshahi Medical College & Hospital, Rajshahi to determine the outcome of conservative ADSBO management, 72 percent of the 100 patients admitted responded to conservative management, 11 percent developed strangulation, and 17 percent failed conservative management. The cautious management team took 72 hours to declare failure. In this study, 72.36 percent of first-attack cases were completely responded. Similarly, 70% of 2nd attack cases and 75% of 3rd attack cases responded conservatively [9]. In a retrospective study done at Mackay Memorial Hospital, Taipei, Taiwan done to evaluate the how long can a patient with conservative management of adhesive bowel obstruction can tolerate; 293 admitted, 220 (75%) put on medical management and 73 operated. The period of observation in patients managed medically ranged from 2 to 12 days (average: 6.9 days), while for those who underwent surgery, the range was 1 to 14 days (average 5.4 days). At surgery, adhesions were the only finding in 46 cases, while there were intestinal complications in 27, or 9.2 % of all 293 admissions. Fever and leukocytosis greater than 15 000/mm3 were predictor of intestinal complications [10]. In a prospective study conducted at the Jammu government medical college and hospital, the non-operative management outcome of a patient with an ADSBO diagnosis was determined. In a group of 60 patients who were admitted and started on conservative treatment, 48 responded to non-operative care, while 12 required surgeries [14]. In 1-year retrospective study done in Tribhuvan University Teaching Hospital, Kathmandu, Nepal to assess the rate of conversion to operative treatment and overall outcome in patients with diagnosis of partial ADSBO, a total of 30 patients was reviewed and conservative treatment was successful in 22 patients (73.3%) average period of 2 days followed by discharge on fourth day of admission. 8 patients (26.6%) were operated for failed conservative management [11]. In a 1-year prospective study done in College of Medical Sciences, University of Calabar, South Nigeria to assess prevalence of acute Intestinal obstruction from post-operative adhesions in a tertiary health facility among 46 cases of small bowel obstruction 11(23.9%) was from ADSBO which is only second to strangulated/incarcerated external inguinal hernia (65.2%). Among all ADSBO cases 63.6% were treated surgically while the remaining 36.4% were managed conservatively with satisfactory outcome [12]. An open randomized controlled clinical trial was conducted at Mulago National Referral and Teaching Hospital, Uganda to compare efficacy of Gastrografin with standard conservative treatment in management of adhesive small bowel obstruction. 50 recruited patients were followed up and analyzed; 25 for each group. Gastrografin group, 22 (88%) patients had relief of obstruction following the intervention, with 3 (12%) requiring surgery. The conservative treatment group had 16 (64%) patients relieved of obstruction. In a study conducted at Nekemte referral hospital in Ethiopia to assess the causes and outcomes of small intestinal obstruction, adhesive small bowel obstruction was found to be the leading cause of small bowel obstruction (35.1 percent), followed by small bowel volvulus (24.2percent) [12]. According to an article published in Qatar by Syed Muhammad Ali, Gastroenterology and Digestive System editor, factors suggesting cancellation of NOM include obstruction lasting more than 72 hours, > 500 ml of NGT aspirate, peritonitis or ischemia as indicated by exacerbation of pain, CRP > 75 mg/l, WCC 10,000/ mm3, and free intra-peritoneal fluid > 500 ml [15]. The prevention and treatment ADSBO are often characterized by surgeons’ personal preferences rather than standardized evidence-based protocols. According to bologna guidelines 2017 minimizing surgical trauma (laparoscopic), using bipolar electro-cautery and ultrasonic devices over mono-polar cautery and using adjuvant adhesion barriers are recommended to reduce the risk of adhesion formation [1]. There is a large amount of conflicting and low-quality evidence in publications regarding treatment of adhesive small bowel obstruction [2].
Objective
General objective
To assess the outcome of conservative management of adhesive small bowel obstruction and associated factors at SPHMMC, Addis Ababa Ethiopia, 2022.
Specific objective
- To assess the success rate of conservative management of ADSBO.
- To assess factors affecting conservative management outcomes.
Research Methods and Materials
Study design
Institution-based cross-sectional analytic study was conducted.
Study area and period
The study was conducted in SPHMMC, a teaching hospital for both undergraduate and postgraduate students located in Addis Ababa, the capital city of Ethiopia. It’s one of the largest hospitals in Ethiopia which currently has 750 inpatient beds. Averagely 500,000 patients are served annually (inpatient and outpatient), with a catchment population of 5 million. In the surgical department there is a total of 40 beds, 9 emergency and 31 elective beds and on average 5000 surgeries are performed annually.
Source population
All patients with a clinical diagnosis of ADSBO admitted to SPHMMC ward or EOPD in the time period April 1/2016 to August 1/2022.
Study population
All patients who are admitted to SPHMMC surgical ward or emergency with a diagnosis of ADSBO and put on conservative management.
Inclusion criteria
All patients with a diagnosis of ADSBO, admitted to SPHMMC surgical ward or EOPD and managed conservatively in a time period between April 1/2016 to August 1/2022.
Exclusion criteria
- Patients who are admitted for conservative therapy and then operated on within 24 hours.
- Patients who were managed non-operatively and discharged improved and returned.
- Charts with insufficient documentation – 15% missed data was disqualified.
- The patient’s age is less than 14 years old.
Sample size
The sample size was calculated by using single population proportion formula by taking proportion of ADSBO as cause of SBO 35% according to a study done in Nekemte referral hospital in Ethiopia with 95% confidence interval at α 0.5 with margin of error of 0.05.
n = Z (α/2)2 * P (1-P)/ d2
Where; n = sample size
- Z α/2 = desired confidence interval 95%, z = 1.96
- P – Prevalence of adhesive small bowel obstruction taken as (0.35), from a study done at Nekemte referral hospital Ethiopia [14].
- d = margin of error (5%)
As a result, the calculated sample size was 350, with 10% of the overall sample size serving as a non-respondent, bringing the total sample size to 385 for the completion of this study. The research population was smaller than the sample size estimated, the entire study population was analyzed which is 183.
Study variable
Dependent variables
- Outcome of conservative management of ADSBO
- Successful outcome
- Non favorable outcome (failure)
Independent variables
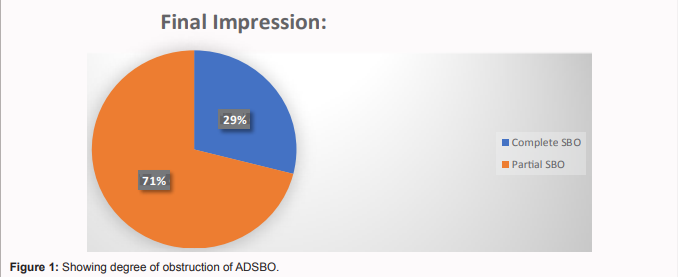
Sex, age, comorbidities, smoking, alcohol, previous small bowel attack, peritonitis in previous lap, type of surgical procedure performed previously, bowel resection and anastomosis in previous procedure, impaired mentation, WBC at admission and final impression of having complete or partial small bowel obstruction.
Data collection
A standardized data extraction checklist was used to collect data from a patient’s chart, which was filled out by trained data collectors (2 medical interns). For any challenges, data collectors were closely supervised by a coordinator. The data extraction format was divided into three sections: socio-demographic factors, clinical profiles of patients, and management information.
Data processing and analysis
Data were entered into Epi-Data version 4.6 and exported to SPSS version 26 software for cleaning, coding, and further analysis. We used descriptive statistics like frequency, mean, and proportion to present participants’ characteristics. Binary logistic regression analysis was fitted, and variables having a p-value of ≤0.25 in bivariable logistic regression were included in the multivariable logistic regression analysis. In the multivariable logistic regression analysis, a p-value of <0.05 with a 95% CI for the adjusted odds ratio was used to declare significant association between the outcome variable and independent variables.
Operational definition
Successful outcome
Complete resolution of sign and symptom of obstruction with conservative management.
Non favorable outcomes/ failure
It’s failed conservative management (persistent signs and symptoms of obstruction despite conservative management) or development of sign and symptoms of strangulations during conservative management.
Incomplete documented charts
If more than 15% of data to be extracted is lost.
Ethical consideration
Written ethical approval was obtained from SPHMMC institutional review board. The identity of the patient was removed. Any degree of data management was kept confidential, and data gathered wasn’t accessed by anyone other than the principal investigator.
Result
Socio-Demographic analysis
A total of 250 patient charts were collected and only 183 cases were found to full fill the inclusion criteria. From 183 cases, 110 (60.1%) were men and 73 (39.9%) were women making the male to female ratio 1.6 to 1. The median age was 45 years and 126 (68.9%) of the patients live in the urban area while 57 (31.1%) come from rural areas. Duration of symptoms in hours, guarding at admission, tenderness, and signs of intra-abdominal collection were considered. Smoking history was in 12 (6.6%) while 16 (8.7%) have alcohol intake history. From the total patient numbers, only 33 (18%) people had some co-morbidity (Table 1) with the commonest being DM followed by HTN and both combined.
Treatment information analysis
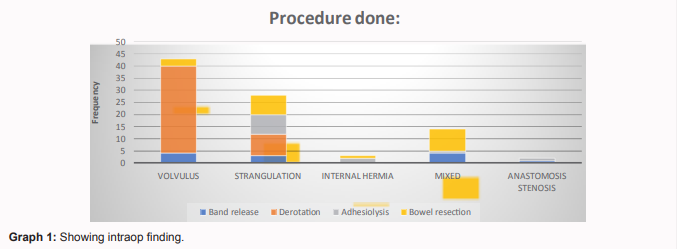
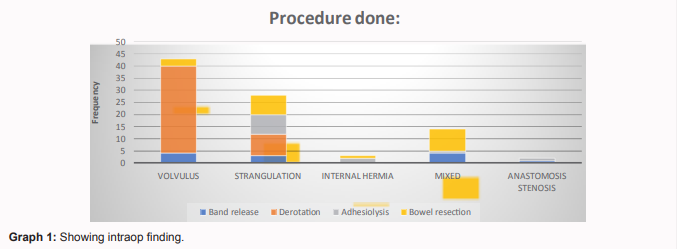
From 183 patients managed conservatively, 93 (51%) had successful outcome and stayed a mean average of 4.71 days. The remaining 90 (49%) patients had failure of resolution after 72 hours or clinical deterioration rendering the conservative management unsuccessful 20 and 29% respectively, resulting in operative management. The length of stay was assessed and it was found to be 8.78 and 13.48 respectively for failure to resolve at 72 hrs and clinical deterioration during conservative management respectively.
Discussion
Intra-abdominal adhesions related to prior abdominal surgery account for up to 75% of cases of small bowel obstruction. Initial management of choice is conservative unless patient has signs of strangulation. From 183 patients managed conservatively, 93 (50.8%) had successful outcome and stayed a mean average of 4.71 days. 49.2% of the remaining patients had failure of resolution after 72 hours or clinical deterioration rendering the conservative management unsuccessful and resulting in operative management. The length of stay was assessed and it was found to be 4.71, 8.78 and 13.48 days respectively for successful, failure to resolve at 72 hrs. and clinical deterioration during conservative management respectively. This is comparable with a retrospective study done by Mu, Jian-Feng et. al. among 288 patients 122 patients (42.3%) underwent operative management while 166 (57.6%), received conservative management (15). In study done UK to analyze ADSBO treatment patterns and associated costs in 110 hospital admissions the mean (SD) length of stay for surgical treatment was 16.3 days (11.0 days) and 7.0 days (4.6 days) for conservative treatment which is different from our study (4). Although it lacks specificity leukocytosis is one of the signs of having ischemia. The severity of ischemia is directly related to the level of leukocytosis. In this study one of the predictors of failed conservative management was having WBC > 11k at time admission having p-value of 0.004 recording an odds ratio of 0.857 (CI 0.38-0.533) supported by the study done by Mu, Jian Feng to assess clinical factors associated with strangulation leukocytosis with WBC greater than 10k was associated with increased risk of strangulation. Specifically, leukocytosis with WBC > 15k was significantly associated with strangulation with p-value of 0.016 AOR 4.31 (CI 1.31–14.16)(15)(16). Type of procedures done known to affect the incidence of adhesion and subsequent adhesive obstruction. Pelvic surgeries of either gynecologic or colorectal surgeries are associated with higher incidence of adhesive small bowel obstruction [1],[4],[16]. In a study to assess burden of adhesion the incidence of ADSBO following lower GI surgeries was found to be 3.2% (2.6% to 3.8%; I2=84%) [2]. In retrospective review conducted to assess small bowel obstruction following colonic surgery the risk of adhesive SBO within 1 year of colectomy is 11 per cent, increasing to 30 per cent at 10 years. Among fifty-six patients admitted to the hospital for ADSBO following previous colorectal surgery eighteen patients were treated conservatively (32 per cent) and 38 underwent laparotomy (68 percent) which shows that the patient who has colorectal index surgery has increased risk of having operative management of ADSBO [17]. In our study among 7 patients who have colorectal procedures as index surgery 5(71.4%) have failed outcome while only 2 have successful management for conservative management also on multivariate logistic regression done having previous procedure of colorectal surgery has significant association with failed conservative management with p-value 0.015 with AOR 0.983(CI 0.001-0.455). Some studies recommend to have early surgical intervention for a patient who has previous low abdominal operation because it’s associated with a poor likely hood of having resolution with conservative management. In a study done in Nigeria, by Dr D.O. Irabor among 52 patients admitted with ADSBO 21 needs operative management, about 62 % of these patients have previous gynecologic procedures(18). In our study also gynecologic surgery was found significantly associated.
with failed conservative management with p-value 0.024; AOR 0.040 (CI 0.002-0.659). Generally low abdominal surgeries have adhesive obstruction which is not amenable for tube decompression which leads to increased risk of failed conservative management. Physical examination solely is found to be less sensitive for identification of strangulation in adhesive small bowel obstruction. Even a very experienced hand the sensitivity of physical examination to pick strangulation is 48% [19]. In a setup where advanced investigative modalities like CT scan isn’t available meticulous physical examination is highly important. In our study tenderness at presentation has significant association with failed conservative management with p-value 0.021, AOR 0.619 (CI .168-.863). Timely surgical intervention is recommended once a patient on conservative management of ADSBO has tenderness on examination. In a study done to develop predictive model for surgery in patients who are on conservative management for ADSBO, presence of intra-abdominal collection was found to be predictive of a need for operative management with p-value of 0.001 AOR 5.2 (CI 1.9–14.2) [20]. In the above study, intra-abdominal collection was one of the 3 major predictive factors for ADSBO patients who were on conservative management which likely need operative management. In our study, signs of intra-abdominal collection at admission was associated with failed conservative management with p-value of 0.031; AOR 0.38 (CI 0.159-0.916). Female sex was significantly associated with successful conservative management outcome with p-value of 0.0004; AOR 5.07 (CI 2.03 -12.67). In this study of total 73 female patients, 65.6% of cases responded to conservative management while the rest needed operative management. This is supported by the study carried out in the department of surgery, Rajshahi medical college hospital by Dr. Md. Mohibul Hassan and et.al among 64 female patients where 78.12% responded to conservative management while 21.88% needed operation, but still had better response than female patients in our setup [9].
Limitation of the Study
The data source was secondary data and pages of charts was lost; some data was incomplete which forced the omission of some cards. The study was a retrospective study.
Conclusion
ADSBO is common and conservative management is the first line of management. Health care givers should take strict follow up during conservative management. In our study, special attention should be given to patients who have leukocytosis (WBC >11K), previous gynecologic and colorectal surgery, signs of collection, and tenderness because they are highly likely associated with failed conservative management. While female gender is associated with successful conservative management.
Recommendation
Adhesive small bowel obstruction is increasing in prevalence in developing countries and it needs to be given attention, and further studies should be done with better design and resources. A multi-institutional study should be done to cross-validate this result in different patient populations.
References
-
1.
Catena F, Di Saverio S, Kelly MD, Biffl WL, Ansaloni L, Mandalà V, et al. Bologna Guidelines for Diagnosis and Management of Adhesive Small Bowel Obstruction (ASBO): 2010 Evidence-Based Guidelines of the World Society of Emergency Surgery. World J Emerg Surg [Internet]. 2011;6(1):5.
-
2.
Richard PG, Issa Y, Van Santbrink EJP, Bouvy ND, Kruitwagen RFPM, Jeekel J, et al. Burden of adhesions in abdominal and pelvic surgery: Systematic review and met-analysis. BMJ [Internet]. 2013;347(7929):1–15.
-
3.
Attard JAP, Maclean AR. Adhesive small bowel obstruction: Epidemiology, biology and prevention. Vol. 50, Canadian Journal of Surgery. 2007.
-
4.
Broek RPG, Krielen P, Di Saverio S, Coccolini F, Biffl WL, Ansaloni L, et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO). World J Emerg Surg [Internet]. 2018;13(1):13–24.
-
5.
Hajibandeh S, Hajibandeh S, Panda N, Khan RMA, Bandyopadhyay SK, Dalmia S, et al. Operative versus non-operative management of adhesive small bowel obstruction: A systematic review and meta-analysis. Int J Surg [Internet]. 2017;45:58–66.
-
6.
Sebastian-Valverde E, Poves I, Membrilla-Fernández E, Pons-Fragero MJ, Grande L. The role of the laparoscopic approach in the surgical management of acute adhesive small bowel obstruction. BMC Surg. 2019;19(1):1–7.
-
7.
Di Saverio S, Birindelli A, Broek R Ten, Davies JR, Mandrioli M, Sallinen V. Laparoscopic adhesiolysis: not for all patients, not for all surgeons, not in all centres. Updates Surg [Internet]. 2018;70(4):557–61.
-
8.
Menzies D, Parker M, Hoare R, Knight A. Medical audit obstruction due to postoperative adhesions: treatment patterns and associated small bowel hospital admissions. 2001;40–6.
-
9.
Hassan M, Paul SC, Sarkar A, Sarker S. Outcome of conservative approach in the management of postoperative adhesive small bowel obstruction. 2019;18(3):32–6.
-
10.
Shih SC, Jeng KS, Lin SC, Kao CR, Chou SY, Wang HY, et al. Adhesive small bowel obstruction: How long can patients tolerate conservative treatment? World J Gastroenterol. 2003;9(3):603–5.
-
11.
Niyaf A, Bhandari R, Singh K. Management of adhesive intestinal obstruction. J Inst Med. 2011;32(2):22–5.
-
12.
O.E. Ngim OEN. Acute Intestinal Obstruction from Post Operative Adhesions in a Tertiary Health Facility, South-South, Nigeria: A one year prospective study. IOSR J Dent Med Sci. 2013;7(2):40–3.
-
13.
Timothy Kimuli PAO. Efficacy of Gastrografin® Compared with Standard Conservative Treatment in Management of Adhesive Small Bowel Obstruction at Mulago National Referral Hospital. J Clin Trials. 2013;03(04).
-
14.
Jemere T, Getahun B, Tesfaye M, Muleta G, Yimer N. Causes and Management Outcome of Small Intestinal Obstruction in Nekemte Referral Hospital, Nekemte, Ethiopia, 2017. Surg Res Pract. 2021;2021:1–6.
-
15.
Mu JF, Wang Q, Wang SD, Wang C, Song JX, Jiang J, et al. Clinical factors associated with intestinal strangulating obstruction and recurrence in adhesive small bowel obstruction: A retrospective study of 288 cases. Med (United States). 2018;97(34).
-
16.
Catena F, Di Saverio S, Coccolini F, Ansaloni L, De Simone B, Sartelli M, et al. Adhesive small bowel adhesions obstruction: Evolutions in diagnosis, management and prevention? World J Gastrointest Surg. 2016;8(3):222.
-
17.
Nieuwenhuijzen M, Reijnen MMPJ, Kuijpers JHC, Van Goor H. Small bowel obstruction after total or subtotal colectomy: A 10-year retrospective review. Br J Surg. 1998;85(9):1242–5.
-
18.
Iasu YT, Kebede T. - 9990 East Cent. Afr. J. surg. (Online). 2012;17(1):70–6.
-
19.
Cho YJ, Park IS, Kim J, Cho HJ, Gwak GH, Yang KH, et al. Factors predicting the need for early surgical intervention for small bowel obstruction. Ann Coloproctol. 2020;36(4):223–8.
-
20.
Komatsu I, Tokuda Y, Shimada G, Jacobs JL, Onodera H. Development of a simple model for predicting need for surgery in patients who initially undergo conservative management for adhesive small bowel obstruction. Am J Surg. 2010;200(2):215–23.